48uep6bbphidvals|341
48uep6bbph|2000F98CTab_Articles|Fulltext
Pancreatic cancer is a leading cause of death in the developed countries. In India the incidence of pancreatic cancer is low (0.5-2.4 per 100,000 men and 0.2-1.8 per 100,000 women).[1] TGF, CA 19-9, CEA, VEGF are amongst of the several tumor markers available for diagnosis and prognosis of the mass lesions of the head of pancreas.[2] When combined (CA-19.9 and CEA),they have a specificity of 95% in detecting pancreatic cancer.[3] A CT-Scan examination is used to find out the extent, local and distant spread of the disease and is used for preoperative staging of the disease. However, sensitivity and specificity of CT imaging in detecting involvement of lymph nodes and peritoneal disease is low.[4]
Apart from diagnosing the tumor, the tumor markers CA 19-9 and CEA are also useful for (i) indication of prognosis, (ii) assessment of therapeutic efficacy, and (iii) detection of residual or recurrent cancer. According to the American Cancer Society, for all stages of pancreatic cancer combined, the one-year relative survival rate is 20%, and the five-year rate is 4%. After Whipple’s surgery and in the absence of nodal involvement the 5-year survival of the patients is 48%.[5] It becomes important to identify patients with advanced disease at the time of diagnosis, as these patients are unlikely to benefit from major surgical intervention and will benefit from palliative treatments like the neo-adjuvant therapy and endoscopic surgeries.[6] This study was conducted to evaluate the role of these tumor markers beyond their routine use of diagnosis, in predicting the operability, survival and recurrence in cases of pancreatic
tumors.
Materials and Methods
This study included 49 patients with pancreatic cancer who were admitted in the Department of Surgical Gastroenterology, Seth G.S Medical College and KEM Hospital, Mumbai, a tertiary care centre with a high patient load. The study lasted for 2 years and also included the patients who have been operated as early as 2007-08 and have been followed up. Patients with obstructive jaundice diagnosed to have exocrine pancreatic cancers and patients diagnosed with a pancreatic malignancy due to any other presenting complaints were included in the study.
Levels of CA-19-9 and CEA were obtained as a part of the investigations carried out in the patients pre-operatively during their hospital stay. CECT-Scan examination to find out the location, boundaries, extent of the tumor and to determine operability was done as a part of the pre-surgical investigations in all patients. The staging of the cancer was then done on the basis of the CECT-scan findings by a senior radiologist.
Criteria for non-resectability on CT-Scan4 included:
· Peritoneal metastases
· Liver metastases with/or ascites
· Extra-pancreatic invasion of adjacent tissues and organs other than the duodenum or bile duct
· Occlusion or stenosis or thrombosis of the major pancreatic vessels
· Encasement of the portal vein was not considered a deterrent to attempted curative surgery, provided that less than half of the vessel circumference and less than 1 cm of its length were affected.
A senior experienced surgeon decided the resectability of the tumors during surgery. Pancreatico-duodenectomy with reconstruction surgery for resection of the tumor was done in resectable cases. A palliative surgery as required or endoscopic stenting was done in non-resectable patients. Postoperatively tumor markers were repeated at every 3 monthly follow up.Levels of tumor markers (pre and post operatively) in both cases- resectable and non-resectable according to the CT-Scan were recorded. CA 19-9 and CEA levels were done for all the patients preoperatively and then at every 3 monthly follow-up.
The normal levels of CA-19-9 were 0-37 U/ml and CEA were 0- 2.5ng/ml. The levels of CA-19-9 and CEA were more than twice are considered to be significant for the prediction of inoperability.[7]The primary objectives were :to evaluate the predictive value of CA19-9 and CEA (two times normal) in determining the inoperability of pancreatic malignancy and to evaluate the predictive value of Ca19-9 and CEA (three times normal) in determining inoperability in radiologically resectable pancreatic malignancy. The secondary objective was to evaluate the survival in patients based on the levels of the tumor markers The data was analyzed with the help of Microsoft excel and Graph pad for statistical analysis. Fischer’s exact test was used for statistical analysis.
Results
A total of 49 patients were analyzed in the study of which 25 patients were non-resectable and 24 were resectable, ( Male : female ratio being 3:1, age range:38-70 years) with mean age being 55 years and mean survival of resectable patients was 2.6years. (range:1 – 3.7years).
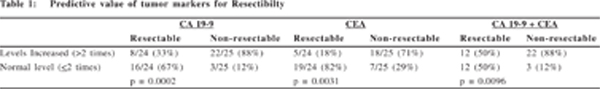
In non-resectable patients, levels of tumor markers CA-19- 9 and CEA were increased in 22/25 (88%) and only 3/25 (12%) patients had normal levels. The markers were elevated in 12/24 (50%) patients who were resectable whereas the other 12 patients had normal levels. This was statistically significant with p-value being 0.0096. This suggests that CA-19-9 and CEA levels predict the inoperability in pancreatic cancers (Table 1).
22/25(88%) non-resectable patients had elevated CA 19-9 levels (>2 times) and 20 out of these 22 patients had CA 19-9 levels(>3 times). 8/24(32%) resectable patients had elevated CA 19-9 levels (>2 times).7 of them had the levels ranging from (106- 350 U/ml) and 1 patient had the value above 1000 U/ml. 16/24(67%) resectable patients reported levels of CA-19-9 (<2 times). This result was also statistically significant (p= 0.0002) establishing the predictive value of elevated levels of CA 19-9 in determining inoperability (Table 1).
18/25 (71%) non-resectable patients and 5/24 (18%) resectable patients had an elevated level of CEA (>2 times) as compared to 19/24 (82%) resectable patients reported a normal level of CEA. Elevated levels of CEA are predictive in determining the inoperability as this result was also found to be statistically significant (p= 0.0031) (Table 1).
Out of the 29 patients who were predicted to be resectable on CT-Scan findings, 24 of them were resectable surgically. 5 patients were non-resectable on exploration. 5/5(100%) had elevated CA 19-9 levels (>3 times). 4/5(80%) patients had a CEA levels (>3 times). The patients were found to be nonresectable due to micro-metastasis in the liver which were <1mm and were not detected on CT-Scan. Some patients also had sub-diaphragmatic seedlings (Table 2).
22 patients who underwent curative were followed up at 3, 6, 9months, 1 year and more than 1 year period. 21/22 (95.5%) of the patients reported a CA-19-9 level less than the significant limits in a period of 3 months and 100% patients reported CA- 19-9 levels below the significant limits at a 9 month period. 1/22 had CA 19-9 level of 297U/ml at 3 months. The level was showing a declining trend (pre-operative – 505U/ml) and reached normal levels at 6 month follow-up. 20/22 (91%) of the patients reported a CEA level less than the significant limits in a period of 3 months and 100% at 9 month period. None of them reported any evidence of an increase in the level of the tumor markers on follow up. 1 patient did not report for follow up at 6 months and 6 patients did not report at 1 year (Table 3).



24 non-resectable patients were followed up at 3, 6, 9 months, 1 year. 23% (5/21) patients with CA 19-9 levels >2 times reported at 1 year follow up. 14% (3/21) patients with CA 19-9 levels >3 times reported at 1 year follow up. All 12 patients with CA-19-9 levels >1000U/ml failed to report at 1 year follow up. Out of them 7/12 (58%) patients failed to report at 6 month follow up and 8/12 (84%) patients did not report at the 9 month follow up. Patients with elevated tumor marker CA-19-9 seem to have a dismal survival as only 1/21 (4.9%) survived for more than a year (Table 4). 14/24 of these had CEA levels >3 times. 3/ 17 patients (17.6%) with CEA levels >2 times and 3/14 (21.1%) with CEA levels >3 times reported at 1 year follow up.
Discussion
Pancreatic malignancies present a significant challenge in both diagnosis as well as the treatment. The tumor markers are effective in clinical monitoring post-surgery or during chemotherapy. Sensitivity of CA 19-9 for the detection of pancreatic cancer ranges in various studies from 67 to 92% with specificities ranging from 68 to 92%.[8,9]In our study, 24 patients were found to be non-resectable. 21/24 patients (88%) had elevated levels of CA19-9 ( p= 0.0002 ). 17/24 (71%) had elevated levels of CEA ( p =0.003). This suggested that elevated levels of CA 19-9 and CEA (>2 times) predicted inoperability in patients of pancreatic cancer.
Some other studies have similarly shown if high levels of CA 19-9 are taken, the specificity of this tumor marker rises over 90% indicating extended disease. CA 19-9 has been reported to be able to predict resectability of pancreatic cancer. According to these studies however, marked elevation of serum CA 19-9, but not CEA, was seen to be associated with advanced and unresectable periampullary cancers.[10]
MDR-CT is the most widely available and best validated tool for pancreatic imaging. CT criteria for nodal involvement include increased size, abnormal shape, loss of fat within the lymph node hilum, and central low attenuation. However, sensitivity and specificity of CT imaging in detecting involvement of lymph nodes is low.[5] CT scan has high sensitivities of detecting invasion of local vessels and metastatic spread. However it is not the best modality for the detection of peritoneal disease.
In our study, of the 49 patients analyzed, 25 patients were found to be non-resectable on surgery.20/25 patients were nonresectable on the basis of CT scan findings also. However, 5/ 25 patients were resectable as per CT scan findings. 5/5 (100%) had CA 19-9 levels (>3times) and 5/5 (100%) had CEA levels (>3 times). 5/5 (100%) had CA 19-9 levels (>2times) and 4/5 (80%) had CEA levels (>2 times). In our study, we observed that CA 19-9 and CEA levels >2 times and >3 times predicted inoperability even in patients which were deemed resectable on CT scan.
It showed that in such patients, a diagnostic laparoscopy would be of benefit to pick up evidence of metastasis which may have not been picked up on the CT-scan. Then if the patient is concluded to be non-resectable a palliative endoscopic surgery can be performed and an exploratory laparotomy avoided.
When compared with staging at exploratory laparotomy, laparoscopic staging with palliative endotherapy offers reduced surgical morbidity, decreased hospital stay, shorter recovery time, and less time to administration of adjuvant therapy. There have been some other studies which have showed that laparoscopy identifies intra-abdominal disease unappreciated by other staging. [11] They have similarly suggested that the patients with resectable disease on CT scan with elevated CA19-9 level may be used as a selection criterion for diagnostic laparoscopy. Experts from Fox Chase Cancer Center recommend laparoscopy for patients who are being considered for resection if the CA19-9 level is greater or equal to 100 U/ml. [12] However studies have not shown elevated CEA levels as a predictor of inoperability in such cases.
In our study, out of 24 resectable patients, 7/22 had levels of CA19-9 (>2 times). 1/7 patients reported elevated CA-19-9 levels at 3 months follow up. However the levels of CA 19-9 in that patient was showing a declining trend and with normal levels at 9 month follow up. All the other patients reported normal levels of CA-19-9 at 9 month follow up. Out of the 24 resectable patients, 4/24 patients had levels of CEA (>2 times).
Of these 2/4 patients had elevated levels at 3 month follow up. Both these patients were showing a declining trend in the CEA levels. However all of them had normal levels at the 9 month follow up. There was no evidence of recurrence in any of the patients despite having elevated levels of tumor markers preoperatively.
Of the 25 patients who were non-resectable in our study, 22/25 had levels of CA 19-9 (>2 times), 20/25 had CA 19-9 levels >3 times and 12/25 of them had CA 19-9 levels >1000U/ml. Only 5/21(23%) patients with levels of CA 19-9 > 2 times followed up at the end of one year, compared to 3/19(14%) patients with levels >3 times. None of the 12 patients with CA 19-9 levels more than 1000U/ml survived for a year.
Similarly, 17/24 non-resectable had elevated levels of CEA (>2times) and 14/24 had levels >3 times. Of these each group of patients, 3/17(17.6%) and 3/14(21%) patients followed up at the end of one year. None of the patients followed up after that. This shows that elevated levels of CEA indicated a poorer survival in non-resectable patients of pancreatic cancer.
In conclusion, elevated levels of CA 19-9 and CEA (>2 times) predict increased chances of inoperability and poor survival in pancreatic tumors. Levels greater than 3 times had increased inoperability even if the patients were deemed resectable on CT-Scan. Diagnostic laparoscopy would be beneficial in these patients. Levels of CA 19-9 (>1000U/ml) indicate a dismal survival in non-resectable group of patients.
References
1. Dhir V, Mohandas KM. Epidemiology of digestive tract cancers in India IV. Gall bladder and pancreas. Indian J Gastroenterol. 1999;18:24–8.
2. Sandblom G Granroth S Rasmussen IC. TPS, CA 19-9, VEGFA, and CEA as diagnostic and prognostic factors in patients with mass lesions in the pancreatic head. Ups J Med Sci. 2008;113:57–64.
3. Nazli O, Bozdag AD, Tansug T, Kir R, Kaymak E. The diagnostic importance of CEA and CA 19-9 for the early diagnosis of pancreatic carcinoma. Hepatogastroenterology. 2000;47:1750–2.
4. Michl P, Pauls S, Gress TM. Evidence-based diagnosis and staging of pancreatic cancer. Best Pract Res Clin Gastroenterol. 2006;20:227–51.
5. Crist DW, Sitzman JV, Cameron JL. Improved hospital morbidity, mortality, and survival after the Whipple procedure. Ann Surg. 1987;206:358–65.
6. Birk D, Beger HG. Neoadjuvant, adjuvant, and palliative treatment of pancreatic cancer. Curr Gastroenterol Rep. 2001;3:129–35.
7. Roche CJ, Hughes ML, Garvey CJ, Campbell F, White DA, Jones L, et al. CT and pathologic assessment of prospective nodal staging in patients with ductal adenocarcinoma of the head of the pancreas. Am J Roentgenol. 2003;180:475–80.
8. Kau SY, Shyr YM, Su CH, Wu CW, Lui WY. Diagnostic and prognostic values of CA 19-9 and CEA in periampullary cancers. J Am Coll Surg. 1999;188:415–20.
9. Schlieman MG, Ho HS, Bold RJ. Utility of tumor markers in determining resectability of pancreatic cancer. Arch Surg. 2003;138:951–5; discussion 955-6.
10. Karachristos A, Scarmeas N, Hoffman JP. CA 19-9 levels predict results of staging laparoscopy in pancreatic cancer. J Gastrointest Surg. 2005;9:1286–92.
11. Luque-de Leon E, Tsiotos GG, Balsiger B, Barnwell J, Burgart LJ, Sarr MG. Staging laparoscopy for pancreatic cancer should be used to select the best means of palliation and not only to maximize the resectability rate. J Gastrointest Surg. 1999;3:111– 7; discussion 117-8.
12. Kim HJ, D’Angelica M, Hiotis SP, Shoup M, Weber SM. Laparoscopic Staging for liver, biliary, pancreas, and gastric cancer. Curr Probl Surg. 2007;44:228–69.