48uep6bbphidvals|335
48uep6bbph|2000F98CTab_Articles|Fulltext
Gastric varices develop in about 20 to 30% of patients with portal hypertension.[1,2,3]The cumulative risk of bleeding from gastric varices has been reported to be 16%, 36% and 44% at 1, 3 and 5 years follow up in patients with cirrhosis.[4] Bleeding from gastric varices (GV) although less common than from esophageal varices, is more severe.[5] Treatment is difficult and the options include surgery (porto-systemic shunts[6] and nonshunt surgeries),[5,7,8] transjugular intrahepatic portosystemic shunt (TIPS)[9] and endoscopic methods.[10,11,12,13] Both surgical and radiological intervention carries significant risk of mortality and morbidity.[14,15,16,17,18[ Endoscopic sclerotherapy using various agents like hypertonic glucose solution, sodiumtetradecylsulfate, ethanolamine oleate and absolute alcohol have been tried in the treatment of gastric variceal bleeding but the results have not been satisfactory.[19,20,21,22]
Tissue adhesive agents (glue) have been used as an alternative to sclerosing agents in the management of bleeding esophageal varices by Gotlib and Zimmerman[23] in 1984 and for gastric varices by Soehendra et al in 1986.[11] N-butyl-cyanoacrylate polymerizes instantaneously and solidifies on contact with blood[24] and is presently used for endoscopic management of gastric variceal bleeding worldwide except in United States. The control of active variceal bleeding has been reported to be 93% to 100% but up to 30% of patients may have recurrence of bleeding on follow up.[25] This procedure has been reported to be safe in small series, but carries a small risk of systemic embolization and is technically demanding.[26]
The aim of the present study is to evaluate the short and longterm efficacy and safety of endoscopic variceal injection of Nbutyl- cyanoacrylate (Nectacryl / Histoacryl) in the management of bleeding gastric varices.
Study Design
Patients
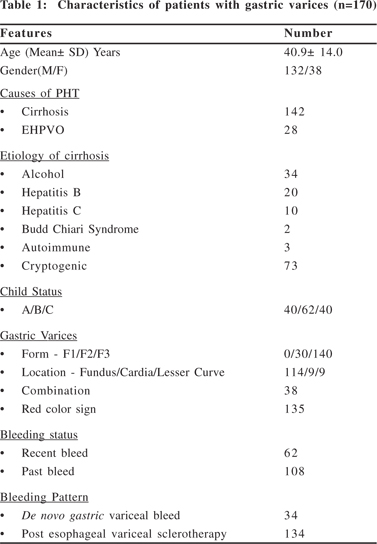
We retrospectively analyzed our endoscopic data of more than 2000 patient who underwent endoscopic treatment for variceal bleeding from 1996 to October 2005. Of these 170 patients underwent endoscopic gastric variceal injection with N-butyl- 2-cyanoacrylate for acute hemostasis or prevention of rebleeding. The mean age was 40.9 + 14.0 (range 13- 69) years;
132 were male. The etiology of portal hypertension was cirrhosis of liver in 142 and extra hepatic portal venous obstruction in 28 patients (Table 1). Most of the patients of cirrhosis had compensated liver function (Child- A 40; B 62; C 40). The etiology of cirrhosis was alcohol in 34, hepatitis B in 20, hepatitis C in 10, Budd-Chiari syndrome in 2 and autoimmune liver disease in 3 each and the remaining 73 did not have any marker positive. As these 73 patients did not undergo anthropometric measurement or liver biopsy or assessment for risk factors for nonalcoholic fatty liver disease, we could not comment whether majority had NAFLD as cause of liver disease. These patients were not investigated with IgG antiHBc or HBV DNA test to rule out occult viral infection. In a study published from our center occult HBV constituted about 10% of cases of cirrhosis.[27] Doppler US was done to evaluate for portal vein thrombosis in all patients. 6 of 142 (4.2%) cirrhosis patients had portal vein thrombosis at initial evaluation. Four patients had recurrence of gastric variceal bleeding due to blocked surgical shunts (interposition porto-caval shunt- 2 and lieno-renal shunt- 2). The gastric varices at endoscopy were classified according to system proposed by Hashizume et al, in respect to the form (F), location(L) and presence of red color signs as this classification includes location and form of gastric varices independent of esophageal varices.[28]Esophageal varices if present were classified grade 1 to 4 according to Conn’s classification[29] and presence of RCS was noted. Most of the varices were large (F3 140 and F2 30), located in the fundus (fundus in 114, lesser curve in 9, cardia in 9, fundus along with lesser curve in 9 and all the three sites in 13) and 135 had RCS. One hundred and thirty four patients were on endoscopic treatment for esophageal varices (grade I-II in 91; 3 in 26 and 4 in 18 patients) at the time of first session of N-butyl-cyanoacrylate injection. One hundred sixteen patients received endoscopic variceal ligation, rest 18 received sclerotherapy using 1% polidoconol initially followed by combined endoscopic treatment (variceal ligation till variceal size decreases to II followed by sclerotherapy) as per our department policy.[30] Majority had grade I-II esophageal varices at the time of first glue injection. Six patients had recurrence of bleed from esophageal varices which was treated with endoscopic sclerotherapy and in these patients rebleeding was presumed to be from esophageal as gastric varix was completely obliterated and stigmata of bleeding was present on esophageal varices.
The bleeding was classified as recent if a) there was active spurt, b) ongoing ooze, or c) fibrin clot seen on the GV or if blood was seen in the stomach in the presence of large gastric varices and no other cause for bleeding could be found. The patients were classified as past bleeder if there was history of upper gastrointestinal bleed in presence of large gastric varices (F2 and F3) with red color signs without any other cause (< grade 2 esophageal varices without stigmata of recent bleed). According to the bleeding pattern the patients were divided in two groups; A. first presentation as gastric variceal bleeding, B. bleeding from gastric varices after successful eradication/ control of esophageal varices by endoscopic band ligation or sclerotherpy. We had 36 and 134 patients in group A and B respectively.
Methods
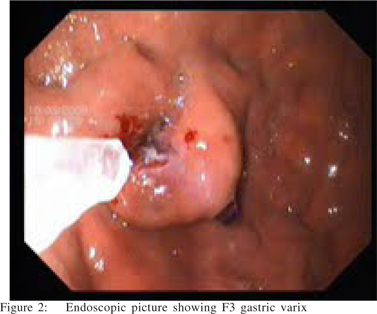
Standard commercial 21-gauge flexible sclerotherapy needle of 8 mm length was used to inject N-butyl-2-cyanoacrylate (Nectacryl; Dr. Reddy’s Laboratories Ltd. Hyderabad, India/ Histoacryl; B.Braun Melsungen AG, Germany) into the gastric varices. A standard forward-viewing video endoscope (EG 2940; Pentax) was used. The tip of the endoscope and the accessory channel were primed with silicone oil before injection to prevent clogging of endoscope during the procedure. The sclerotherapy needle was primed with lipiodol before injection. Glue was mixed with lipiodol in 4:1 ratio and used for injection. The largest of the varices with red color sign was chosen first (Figure 1 &2). After targeting, the needle was taken out from the sheath, a deep puncture of the gastric varix made, and the glue quickly injected followed by flushing of the needle with lipiodol. The volume used was 0.5 to 4ml per aliquot. The amount per injection was decided by size of varix (~0.5ml for F1, 1-2ml for F2 and 2-4ml for F3 varix).[31] Routine upper abdomen radiograph were done after each session to check the presence and contour of glue cast and satisfactory obliteration of feeding vessel (Figure 3). In presence of active bleed from a gastric varix the bleeding point or a site near it was chosen.


Patients underwent repeat endoscopic evaluation after 3 weeks for 3 months then every 3 months up to 1 year then 6 monthly or any time if the patients had recurrence of bleed.Gastric varices were classified as obliterated if they felt to be hard on blunt probing with the needle sheath, and nonobliterated if they appeared compressible and indented on pressure. N-butyl-cyanoacrylate injection was repeated if the patients had recurrence of bleed or had unobliterated varices with or without red color signs. After one recurrence of bleeding the patients were also given the choice of surgical treatment. If the patients had esophageal varices, endoscopic variceal sclerotherapy or ligation was also done at 3 weekly interval till the varices were eradicated.
The outcome assessment included hemostasis for active bleeding which was defined as control of bleeding at 48 hours. The recurrence of bleeding was defined as bleeding arising from the injected or nearby gastric varices after 48 hours. The use of alternative treatment (balloon tamponade or surgery or TIPS) and mortality were recorded. The gastric variceal status at the time of last follow up was recorded. Primary success was defined as absence of recurrent bleeding following N-butylcyanoacrylate injection during the entire period of follow up.
Secondary success was defined as absence of recurrent bleeding following reinjection of N-butyl-cyanoacrylate for first recurrence of bleeding during the entire period of follow up. Definitive hemostasis included both primary and secondary success. Treatment failure was defined as failure to achieve definitive hemostasis by endoscopic N-butyl-cyanoacrylate injection. “The authors affirm that all research related to this study was carried out in accordance with the Helsinki Declaration as revised in 1989”.
Statistics
The results are expressed as mean + standard deviation. Statistical software SPSS 10.0 was used for data analysis. The risk factors for recurrent bleeding including Child Pugh class, age, gastric varix location, number of sessions and volume of glue injection were analyzed by Spearman’s correlation coefficient and Chi Square test. p value <0.05 was taken as significant. Logistic regression analysis was done to analyze the predictive value of Child-Pugh status, initial gastric variceal form and location, volume and number of sessions of N-butylcyanoacrylate injection for recurrence of bleeding from gastric varices in the follow up period. Event curve (recurrence of bleeding) was constructed by Kaplan Meier method for etiology of portal hypertension, Child-Pugh class, bleeding pattern and the difference was assessed by Log rank test.
Results
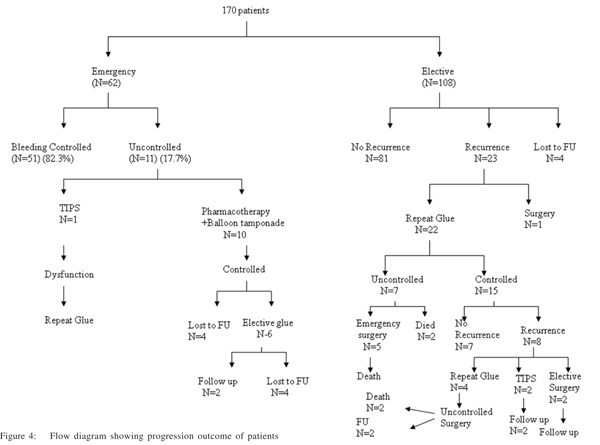
170 patients received N-butyl-cyanoacrylate injection for gastric varices. Of them, 62 underwent glue injection as an emergency procedure to achieve hemostasis from actively bleeding GV and in 108 patients it was done as an elective procedure for prevention of re-bleeding. The 48-hours hemostasis in recent bleeders was 82.3%, (51 out of 62). Among eleven patients who could not achieve 48 hours hemostasis, 1 was taken for emergency TIPS, 10 were managed with pharmacological treatment as they were unfit for surgery. Bleeding was controlled in all of them. Six of the ten who were managed with pharmacological treatment underwent a repeat glue injection electively. Four of the six were lost to follow up (Figure 4). The mean volume of N-butyl-2-cyanoacrylate injected at first injection was 1.4 + 0.6 (range 0.5 to 4) ml.
Among 108 patients who underwent elective glue injection, the initial bleeding was managed with pharmacological treatment in 78 patients at secondary care hospital and later referred to our center. Remaining 30 patients were managed atour hospital with pharmacological treatment as these patients were unfit for endoscopy due to hepatic encephalopathy. The mean time interval between first episode and glue injection was 10.5± 4.2 days (4-30 days).
Of the 170 patients, 12 were lost to follow up after initial endoscopic treatment. The remaining 158 patients had mean period of follow up of 30.7 + 17.2 months (12 to 66 months); 80 patients had follow up for more than 20 months. Total volume injected per varix was 1.6 ± 0.6ml (range 0.5-4 ml) and per patient was 2.5 ± 1.7 ml per patient and mean sessions required for eradication were 1.9±1.0. On follow up, 76 patients underwent repeat sessions of N-butyl-2-cyanoacrylate injection (mean 2.3 + 0.6); the mean cumulative volume of N-butyl-cyanoacrylate injected per patient was 2.8 + 1.6 (0.5 to 8 ml). Before 2004, we used to prepare aliquots of 1ml each and during glue injection there used to be considerable time delay due to exchange of syringes. Now we prepare aliquot according to predefined volume (volume drawn in a single syringe). We used to encounter problems of clogging of needle during injection frequently before 2004. For last 2 years with the above modification needle clogging is rare. During subsequent 2 years we have been able to salvage most needles by immediate flushing with lipiodol after injection.
At the time of last follow up, the gastric variceal status was completely obliterated in 32 (22.6%), F1 and solidified in 46 (32.6%) and F2 and solidified in 64 (45.0%; Table 2). After initial regression 16 (11 %) patients had shown increase in size of gastric varices on follow up.
Bleeding from gastric varices recurred in 23 (14.5%) of 158 patients, 8 of whom had a 2nd recurrence of bleed. The first recurrence occurred after a mean duration of 2.5 (range 1 week to 24) months. Majority of them 69.5% (16 out of 23) had recurrence within 6 months. In ten (45.4%) of the patients the rebleed was due to sloughing of the glue cast and formation of ulcer at the injection site and in the remaining 13 patients it was due to recurrence of large gastric varices as these patients had completely obliterated or solidified varices on follow up and bleeding occurred from varices which were not there at initial valuation and appeared at different site compared to initial varices.
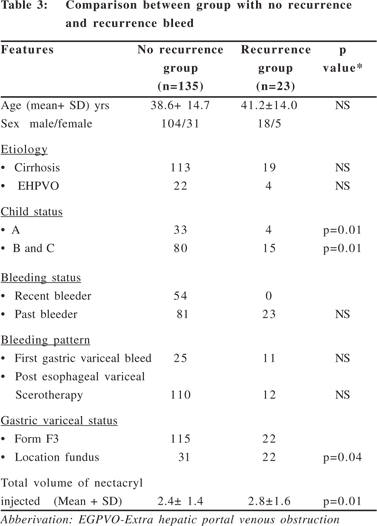
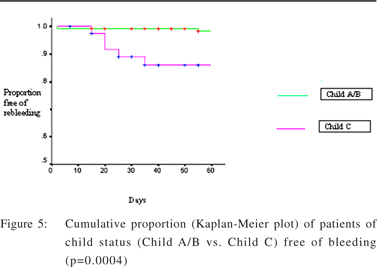
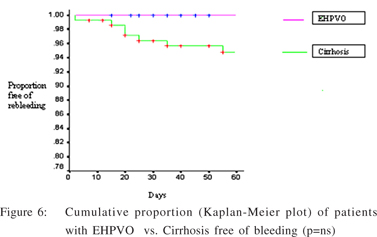
On logistic regression analysis, number of sessions of Nbutyl- cyanoacrylate injection (p =0.04) and Child status (p=0.01) showed statistical significance for recurrence of bleeding. There was significant difference between recurrence of bleed and non-recurrence group of number of sessions of N-butyl-cyanoacrylate injection (p=0.04), total volume of Nbutyl- cyanoacrylate injected (p= 0.01) and gastric variceal location (p 0.043) (Table 3). The Kaplan-Meier event curve (Figure 5 & 6) comparing Child status showed significant overall difference (Log rank test).
We assessed feasibility of TIPS only in those patients in whom initial control of bleeding with glue had failed. Four of 23 patients who had failed endoscopic treatment had portal vein thrombosis and were not candidates for TIPS while in remaining patients TIPS was feasible. Of these 23 patients, 22 underwent repeat N-butyl-cyanoacrylate injection; one was taken up for gastroesophageal devascularization. The 48 hours bleed control following repeat N-butyl-cyanoacrylate injection was 68.1% (15 of 22). Two patients died (8.6%) due to uncontrolled bleeding. Remaining five were taken for emergency devascularization, all five died due to liver failure during postoperative period. Eight patients out of 15 (53.3%) had 2nd recurrence of bleeding within 2 to 12 months following N-butyl- cyanoacrylate injection for first recurrence.
The sloughing of glue cast and ulcer formation was the cause of recurrence in 4 patients. Four of them underwent another session of N-butylcyanoacrylate injection and in all four patients it failed to control the bleeding and they were taken up for shunt surgery. In two pateints, distal splenorenal shunt and in the remaining two patients interposition portocaval shunt was done. Two of them died during postoperative period due to liver failure, remaining two are on follow up. Two patients underwent TIPS as both had poor liver function and unfit for surgery. Both the patients are on follow up with patent TIPS. The remaining two patients after initial bleed control by medical treatment underwent shunt surgery and are on follow up.
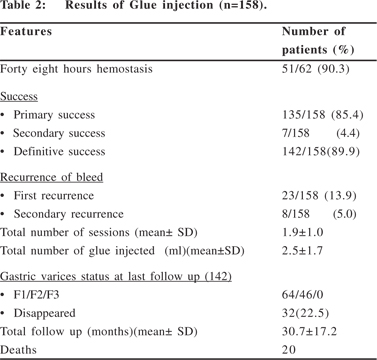
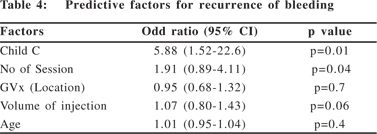
The primary and secondary success was 85.4% (135 out of 158) and 4.4% (7 out of 158) respectively. The definitive success was 89.9% and the treatment failure was 10%. None of the patients had significant complications related to the procedure except for injection site ulceration in 32patients. One of the patients with cirrhosis of liver had one successful pregnancy following one session of N- butylcyanoacrylate injection without any effect in the fetus. During glue injection, few patients complained of chest pain and cough but none of them showed any evidence of glue embolization on chest and abdomen radiographs or additional hospital stay or intervention due to procedure. Total of 20 patients died {uncontrolled gastric variceal bleed-9 (postendoscopic treatment-2, post surgery-7), Liver failure-11}.( Table 4)
Discussion
N-butyl-cyanoacrylate is very effective in controlling active bleeding from gastric varices. The reported success for hemostasis in active gastric variceal bleeding is 90% to 100%.[3,31] The other sclerosants used in previous studies for treatment of gastric varices had poor control and high recurrence of bleed.[19,20,32]Sarin et al have reported use of absolute alcohol as sclerosant for treatment of gastro esophageal varices.[20]They have reported acute hemostasis only in two thirds of the patients and high rebleeding rate of 53% from isolated gastric varices. We have found good efficacy of N- utylcyanoacrylate injection for bleeding gastric varices. The 48- hours hemostasis for recently bleeding gastric varices was 82.3% for the first injection, which is comparable to the published reports.[31,33]We had to reinject the gastric varices for second and third recurrence of bleeding as relatives of the patients were not willing for major surgery. The efficacy of Nbutyl- cyanoacrylate for active bleeding was low in recurrent gastric variceal bleeding. Huang et al reported the success of repeat superglue injection for first recurrence of gastric variceal bleed to be 71.4% (15 out of 21).[31]We achieved 68% (15/22)hemostasis at 48 hours repeat injection of N- butylcyanoacrylate for the first recurrence and 0% for second recurrence. Secondary success rate in our study was 4.4 %( 7/ 158), as defined by absence of recurrent bleeding following reinjection of N-butyl-2-cyanoacrylate for first recurrence of bleeding during the entire period of follow up. This may be due to longer follow up and due poor liver function (as most of them were Child- Pugh stage C).
It is not clear whether the patients with recurrence of bleeding following N-butyl-cyanoacrylate injection should be reinjected. TIPS followed by liver transplant could be a better option if the facilities are available.
The primary, secondary and definitive success in our series was 85.4%, 4.4% and 89.9% respectively. Huang et al have reported primary, secondary and definitive success of 76.6%,16.7% and 93.3% in a recently published study using superglue for the treatment of gastric varices. The mean follow up period in their study was 13.2 + 2.0 months.[31]We had a much longer follow up period of 30.7 + 17.2 months compared to study by Huang et al . This probably explains the lower secondary success rates in our study, because it is known that the rate of rebleeding from varices increases with the length of follow up.[4]
Although N-butyl-cyanoacrylate has a high success rate in hemostasis of actively bleeding varices, the recurrence of bleeding continues to be a problem. In most of the studies the recurrence of bleeding is reported to be around 30%.[31,34]In our series the recurrence of bleeding was 13.9 % (22 out of 158). The first recurrence of bleeding occurred in most patients 77.2% (17 out of 22) within 6 months after the initial N-butylcyanoacrylate injection. N-butyl-cyanoacrylate forms a cast in the varices and blocks it. It can ulcerate and slough out leading to recurrence of bleeding. About 45.5% (10 out of 22) our patients had rebleeding due to ulceration and extrusion of the cast. All our patients were on proton pump inhibitors. We encountered ulcer at injection site commonly, but in these 10 patients with recurrence of bleeding, there was ulcer at injection site with stigmata of recent bleed and no other source of bleeding. We could not find any explanation to more catastrophic bleed in our study as compared to self limited bleed due ulceration as reported by Huang et al.[31]
Huang et al reported post cyanoacrylate injection cast extrusion in 26.6% of patients within a mean period of 6 months.[31] It is not clear whether the volume and site of injection has any influence on formation of ulcers and cast extrusion. Binmoeller and Soehendra suggested that paravariceal injection leads to more ulceration, so the injection should be strictly intravariceal.[24] Majority of the recurrence of bleeding occurred in cirrhosis patients. Various factors like size of varices, underlying disease, portal vein thrombosis and liver function status have been reported as risk factors for recurrence of bleeding.[4] When we tried to compare the patients who had recurrent bleeds from gastric varices with those who did not, poor liver function and fundal location seemed to be associated with a higher risk of rebleed.
The schedule of gastric variceal N-butyl-cyanoacrylate injection varies as there are no definite guidelines in the literature. There can be two approaches following first injection; either re-inject only if the patient rebleeds on demand basis,[34]or re-inject the varices repeatedly on follow up till they are completely obliterated or disappeared.[24,31]There are no randomized studies to show that one approach is better than the other. In a comparative study, Lee et al reported repetitive injection group had significantly reduced rate of late recurrence of bleeding compared to the ‘on demand’ injection group.[34]But, this study was nonrandomized and the two groups were not receiving injection at the same period of time. They have usedendoscopic ultrasound guidance for repetitive injections.
Palpation of varices with blunt sheath of the sclerotherapy needle has been used to assess the obliteration of gastric varices.[24,31]We followed a policy of repetitive injection depending on the size of the varices on follow up endoscopy. The obliteration of varices was assessed by blunt palpation with sheath of sclerotherapy needle.
The dilution of glue and volume injected per session varies in different reported series. We have used sufficient volume of N-butyl-cyanoacrylate to cause hardness of the targeted varix. In different studies authors have also used this agent varying from undiluted to 1:1 to 2:1 dilution with lipiodol.[29,35]The dilution is made to delay the polymerization so that the injector does not get stuck in the solidified varix. Traditional dilution (1:1 or 2:1) of glue with lipiodol has been reported to cause systemic and pulmonary embolization (depends on speed and volume of injection). On the other hand use of undiluted glue frequently causes needle clogging and does not permit radiological visualization of the glue cast to ensure blockage of feeder vessel.[36,37]Our experience with limited dilution of glue (4:1) provided benefit on both these issues. We have not encountered any problem related to quick solidification of Nbutyl-cyanoacrylate or pulmonary embolism with this small amount of lipiodol.
The accompanying esophageal varices require band ligation or sclerotherapy because they also carry the risk of bleeding.[26]We treated the esophageal varices with endoscopic variceal ligation or injection of sclerosant initially followed by combined endoscopic treatment as per our department policy. There have been no reports in literature of use of N-butylcyanoacrylate for prophylaxis of bleeding from large gastric varices. Some of the patients on esophageal variceal sclerotherapy, who develop large gastric varices with RCS on follow up, pose a problem. Whether prophylactic injection of glue into their gastric varices would help is not clear. Some authors have advocated routine injection of glue into large gastric varices detected at the time of esophageal variceal sclerotherapy.[24]We feel this is an unsettled issue which needs to be addressed in prospective trials. There was reduction in the size of gastric varices on follow up after glue injection.
Large F3 varices were present in 82.8% at the initiation of treatment. At the last visit, majority of varices had decreased in size {F2 solidified in (45.0%), F1 solidified in (32.3%)} or had completely disappeared in (22.5%). Most of reported series mention about obliteration (solidification on palpation with blunt sheath of sclerotherapy needle) and not about eradication of gastric varix.[24,31]After initial regression, 11 % of patients showed increase in size of gastric varices during follow up. The decrease in size of gastric varices depends on the policy of N-butyl-2-cyanoacrylate injection. The repeated injection group aims at total obliteration of varices. Lee et al reported > 90% obliteration of isolated gastric varices after 2.2 + 1.7 sessions.
Except for the post injection local ulceration, we have not found any major complications of cyanoacrylate injection. One of our patients had a successful pregnancy without any adverse effect to the fetuses. Safety of cyanoacrylate in control of acute bleeding from gastric varices during pregnancy has been reported.[38] The overall mortality in this study was 12.6% (20 of 158), most of them (11 out of 20) were related to liver failure due end stage liver disease.
In conclusion, the first N-butyl-cyanoacrylate injection is very effective in controlling bleeding from gastric varices. This agent is not so effective for the recurrence of bleeding from gastric varices. Repeated injections are required to obliterate the varices. In long term follow up, N-butyl-cyanoacrylate has a good safety profile. The issues like therapeutic modalities for recurrence of bleed following N-butyl-cyanoacrylate injection and prophylactic endoscopic treatment of large unbled gastric varices with RCS who are already on sclerotherapy program for esophageal varices needs further study.
References
1. Sarin SK, Lahoti D. Management of gastric varices. Baillieres Clin Gastroenterol. 1992;6:527–48.
2. Sarin SK, Lahoti D, Saxena SP, Murthy NS, Makwana K. Prevalence, classification and natural history of gastric varices: A long term follow up study in 568 portal hypertension patients. Hepatology. 1992;16:1343–9.
3. Ryan BM, Stockbrugger RW, Ryan JM. A pathophysiologic, gastroenterologic, and radiologic approach to the management of gastric varices. Gastroenterology. 2004;126:1175–89.
4. Kim T, Shijo H, Kokawa H, Tokumitsu H, Kubara K, Ota K et al. Risk factors for hemorahge from gastric fundal varices. Hepatology. 1997;25:307–12.
5. Rockey DC. Management of gastric varices. Gastroenterology. 2001;120:1875–7.
6. Thomas PG, D’Cruz AJ. Distal splenorenal shunting for bleeding gastric varices. Br J Surg. 1994;81:241–4.
7. Rietoenschneider T, Bermel RE, Hirner A. Results from devascularisation surgery of gastroesophageal junction in the recurrent hemorrhage of esophageal and fundus varices. Zentralb Chir. 1994;119:291–7.
8. Greig JD, Garden OJ, Anderson JR, Carter DC. Management of gastric variceal hemorrhage. Br J Surg. 1990;77:297–9.
9. Barange K, Peron JM, Imani K, Otal P, Payen JL, Rousseau H, et al. Transjugular intrahepatic portosystemic shunt in the treatment of refractory bleeding from ruptured gastric varices. Hepatology. 1999;30:1139–43.
10. Sarin SK, Jain AK, Jain M, Gupta R. A randomized controlled trial of cyanoacrylate versus alcohol injection in patients with isolated fundic varices. Am J Gastroenterol. 2002;97:1010–5.
11. Soehendra N, Nam VC, Grimm H, Kempeneers I. Endoscopic obliteration of large esophagogastric varices with bucrylate. Endoscopy. 1986;18:25–6.
12. Akahoshi T, Hashizume M, Shimabukuro R, Tanoue K, Tomikawa M, Okita K, et al. Long-term results of endoscopic Histoacryl injection sclerotherapy for gastric variceal bleeding: a 10-year experience. Surgery. 2002;131:S176–81.
13. Lo GH, Lai KH, Cheng JS, Chen MH, Chiang HT. A prospective, randomized trial of butyl cyanoacrylate injection versus band ligation in the management of bleeding gastric varices. Hepatology. 2001;33:1060–4.
14. Sugiura M, Futagawa S. Esophageal transection with paraesophagogastric devascularization (the Sugiura procedure) in the treatment of esophageal varices. World J Surg. 1984;8:673–9.
15. Ginsberg RJ, Waters PF, Zeldin RA, Spratt EH, Shandling B, Stone RM, et al. A modified sugiura procedure. Ann of Thoracic Surg. 1982;34:258–64.
16. Triger DR, Johnson AG, Brazier JE, Johnston GW, Spencer EF, McKee R, et al. A prospective trial of endoscopic sclerotherapy v oesophageal transection and gastric devascularization in long term management of bleeding oesophageal varices. Gut. 1992;33:1553–8.
17. Chau TN, Patch D, Chan WY, Nagral A, Dick R, Burroughs AK. “Salvage” transjugular intrahepatic portosystemic shunt: gastric fundal compared with esophageal variceal bleeding. Gastroenterology. 1998;114:981–7.
18. Spahr L, Dufresne MP, Bui Bt, Martinet JP, Fenyves D, Willems B et al. Efficacy of TIPS in the prevention of rebleeding from esophageal and fundal varices: a comparative study. Hepatology. 1995;22:296A.
19. Chang KY, Wu CS, Chen PC. Prospective randomized trial of hypertonic glucose water and sodium tetradecyl sulfate for gastric variceal bleeding in patients with advanced liver cirrhosis. Endoscopy. 1996;28:481–6.
20. Sarin SK, Sachdev G, Nanda R, Mishra SP, Broor SL. Endoscopic sclerotherapy in the treatment of gastric varices. Br J Surg. 1988;75:747–50.
21. Sarin SK. Long-term follow-up of gastric variceal sclerotharapy: an eleven-year experience. Gastrointest Endosc. 1997;46:8–14.
22. Heneghan MA, Byrne A, Harrison PM. An open pilot study of the effects of human fibrin glue for endoscopic treatment of patients with acute bleeding from gastric varices. Gastrointest Endosc. 2002;56:422–6.
23. Gotlib JP, Zimmermann P. Une nouvelle technique de traitement endoscopique des varices oesophagiennes: I’obliteration. Endos Dig. 1984;7:10–2.
24. Binmoeller KF. Glue for gastric varices: some sticky issues. Gastrointest Endosc. 2000;52:289–301.
25. Dhiman RK, Chawla Y, Taneja S, Biswas R, Sharma TR, Dilwari JB. Endoscopic sclerotherapy of gastric variceal bleeding with N-butyl-2-cyanoacrylate. J Clin Gastroenterol. 2002;35:222–7.
26. Binmoeller KF, Soehendra N. The use of histoacryl tissue adhesive for the treatment of variceal bleeding. In: Sivak Jr, editor. Sivak Gastroenterologic endoscopy. 2nd ed. Philadelphia: B Saunders; 2000. p.178–85.
27. Agarwal N, Naik S, Aggarwal R, Singh H, Somani SK, Kini D, et al. Occult hepatitis B virus infection as a cause of cirrhosis in a region with intermediate endemicity. Indian J Gastroenterol. 2003;22:127–31.
28. Hashizume M, Kitano S, Yamaga H, Koyanagi N, Sugimachi K. Endoscopic classification of gastric varices. Gastrointest Endosc. 1990;36:276–80.
29. Conn HO. Ammonia tolerance in the diagnosis of esophageal varices. A comparison of endoscopic, radiologic, and biochemical techniques. J Lab Clin Med. 1967;70:442–51.
30. Lo GH, Lai KH, Cheng JS, Lin CK, Huang JS, Hsu PI, et al. The additive effect of sclerotherapy to patients receiving repeated endoscopic variceal ligation: a prospective, randomized trail. Hepatology. 1998;28:391–5.
31. Huang YH, Yeh HZ, Chen GH, Chang CS, Wu CY, Poon SK, et al. Endoscopic treatment of bleeding gastric varices by N-butyl- 2-cyanoacrylate (Histoacryl) injection: long term efficacy and safety. Gastrointest Endosc. 2000;52:160–7.
32. Memon MA, Jones WF. Injection therapy for variceal bleeding. Gastrointest Endosc Clin of N Am. 1999;9:231–52.
33. Gimson AE, Westaby D, Williams R. Endoscopic sclerotherapy in the management of gastric variceal hemorrhage. J Hepatol. 1991;13:274–8.
34. Lee TY, Chan FK, Ng EK, Leung VK, Law KB, Yung MY et al. EUS-guided injection of cyanoacrylate for bleeding gastric varices. Gastrointest Endosc. 2000;52:168–74.
35. Lo GH, Lai KH, Cheng JS, Chen MH, Chiang HT. A prospective, randomized trial of butyl cyanoacrylate injection versus band ligation in the management of bleeding gastric varices. Hepatology. 2001;33:1060–4.
36. Cheng PN, Sheu BS, Chen CY, Chang TT, Lin XZ. Splenic infarction after histoacyl injection for bleeding gastric varices. Gastrointest Endosc. 1998;48:426–7.
37. D’Imperio N, Piemontese A, Baroncini D, Billi P, Borioni D, Dal Monte PP, et al. Evaluation of undiluted N-butyl-2-cyanoacrylate in the endoscopic treatment of upper gastrointestinal varices. Endoscopy. 1996;28:239–43.
38. Dhiman RK, Biswas R, Aggarwal N, Sawhney H, Chawla Y. Management of variceal bleeding in pregnancy with endoscopic variceal ligation and N-butyl-2-cyanoacrylate: report of three cases. Gastrointest Endosc. 2000;51:91–3.