48uep6bbphidvals|432
48uep6bbph|2000F98CTab_Articles|Fulltext
An 80-year-old male presented with worsening fever, chills
and night sweats 10 days after he received his fifth intravesical
BCG instillation for his recurrent low-grade transitional cell
carcinoma of the bladder. Review of systems was remarkable
for mild dysuria and hematuria. Physical examination revealed
a temperature of 102°F. He had no hepatosplenomegaly or
lymphadenopathy. Laboratory evaluation was significant for
leukopenia (3000/µL) and elevated LFTs (alkaline phosphatase
(ALP)-378 U/L, AST-70 U/L, ALT-26 U/L). Prior to presentation,
isoniazid was initiated by his urologist for presumptive BCG
infection. Rifampin and levofloxacin were added upon
admission to the hospital. Routine blood and urine cultures did not yield any pathogens and the results of serologic tests
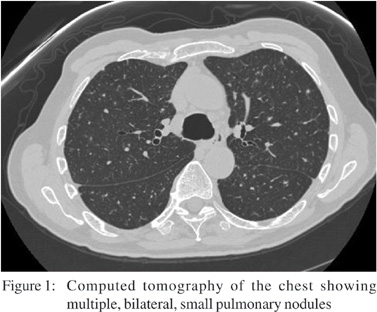
to assess virus, bacteria, and fungus were negative. Chest Xray was unremarkable but the chest-CT revealed diffuse, miliary
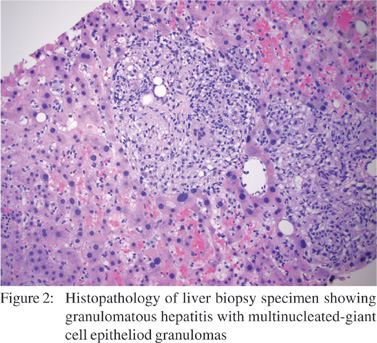
nodular infiltrates suspicious for Mycobacterium infection (Figure 1). A USG-guided liver biopsy was performed for a
persistently elevated ALP and revealed granulomatous hepatitis with non-caseating epithelioid granulomas (Figure
2). Gram stain, AFB, GMS, FITE and immunohistochemical
stains did not detect any organisms and tissue culture was
negative. Worsening pancytopenia prompted a bone marrow
biopsy that revealed multiple large granulomas. The patient gradually improved and his fever subsided within several days of anti-tuberculous therapy. Liver abnormalities resolved during
the following week. He completed a 6-month course of isoniazid
and rifampin, and continues to do well at 1-year follow-up.
Intravesical BCG is an effective treatment for superficial
bladder cancer with a success rate varying between 63 and
100%.[1,2] Minor complications including hematuria, cystitis, fever
(<38.5°C) and malaise are quite common, whereas major
complications such as both local (granulomatous prostatitis,
epididymo-orchitis, ureteral obstruction, bladder contracture)
and systemic reactions (fever >39.5°C, sepsis, pancytopenias,
granulomatous hepatitis and pneumonitis) occur
occasionally.[2,3,4,5]
BCG complications generally result from contiguous and
hematogenous spread of intravesical mycobacteria through
inflamed and/or disrupted urothelium most frequently caused
by traumatic catheterization, bladder perforation, or by
extensive tumor resection.[2,3,4,5] Granulomatous hepatitis is a rare
(<0.4%) and serious complication after BCG instillation, with
unclear pathogenesis.[2,3,4] It has been considered a
hypersensitivity reaction to BCG based on negative staining
and cultures of liver tissue.[2,3,4] However, cases have been
reported in which mycobacteria were present on staining and
mycobacterial DNA was detected in liver tissue suggesting a
liver infection after hematogenous dissemination of BCG, rather
than hypersensitivity.[4]
There have been no prospective studies to evaluate the
optimal treatment for BCG infection.[2,3,4,5] In severe systemic cases,
some data supports the administration of three anti-tuberculous
drugs including isoniazid, rifampin and ethambutol for at least 6 months.[2,3,4] The addition of corticosteroids during initial
therapy may assist in a faster resolution of inflammatory
complications.[2,3,4]
References
- Witjes JA, vd Meijden AP, Debruyne FM. Use of intravesical
bacillus Calmette-Guerin in the treatment of superficial
transitional cell carcinoma of the bladder: an overview. Urol
Int. 1990;45:129–36.
- Trevenzoli M, Cattelan AM, Marino F, Sasset L, Donà S,
Meneghetti F. Sepsis and granulomatous hepatitis after
bacillus Calmette-Guerin intravesical installation. J Infect.
2004;48:363–4.
- Lamm DL, van der Meijden PM, Morales A, Brosman SA, Catalona WJ, Herr HW, et al. Incidence and treatment of
complications of bacillus Calmette-Guerin intravesical
therapy in superficial bladder cancer. J Urol.
1992;147:596–600.
- Leebeek FW, Ouwendijk RJ, Kolk AH, Dees A, Meek JC,
Nienhuis JE, et al. Granulomatous hepatitis caused by
Bacillus Calmette-Guerin (BCG) infection after BCG bladder
instillation. Gut. 1996;38:616–8.
- Gonzales OY, Musher DM, Brar I, Furgeson S, Boktour MR, Septimus EJ, et al. Spectrum of bacillus Calmette-Guerin
(BCG) infection after intravesical BCG immunotherapy. Clin
Infect Dis. 2003;36:140–8.