48uep6bbphidvals|431
48uep6bbph|2000F98CTab_Articles|Fulltext
Introduction
Peristomal pyoderma gangrenosum (PPG) is a rare condition
seen in patients with inflammatory bowel disease. It causes significant morbidity, complicates stomal care and prolongs
the duration of treatment. The management of this condition is difficult and requires a multidisciplinary approach involving
the gastroenterologist, dermatologist, surgeon, and stomal
therapist. We report 2 patients of PPG with severe ulcerative
colitis. Through these cases we attempt to illustrate the varying response these patients may have to high dose steroid therapy
which may necessitate an earlier recourse to completion proctectomy or colectomy.
Case 1
A twenty-one year old man, a known case of chronic steroiddependant
ulcerative colitis, underwent subtotal colectomy with end ileostomy and a Hartmann’s rectal pouch procedure.
Following surgery, the steroids were gradually tapered over a
period of 1 month. Four months following complete withdrawal
of steroids, the patient developed a painful peristomal ulcer (6
cm by 5 cm) (Figure 1a). There were no constitutional
symptoms, hematochezia, or extra-intestinal manifestations.
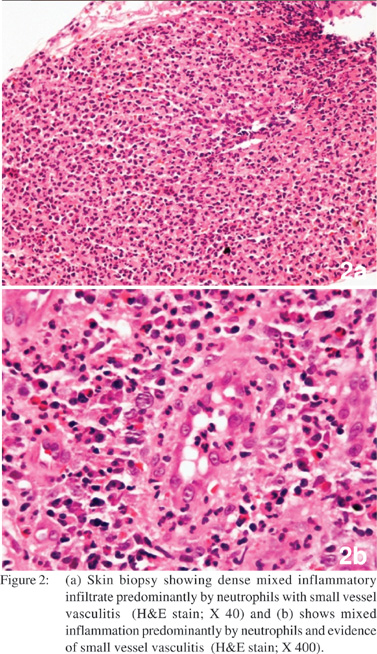
The skin biopsy done showed surface ulceration with dense
mixed inflammatory infiltrate (predominantly neutrophils), and evidence of small vessel vasculitis, with no microorganisms
seen on special stains which was consistent with the clinical
diagnosis of pyoderma gangrenosum (Figures 2a & 2b). The
patient was re-started on oral steroids (prednisolone 40 mg per
day). Within 1 week of starting steroids, the lesions showed
signs of healing (Figure 1b). After 1 month of steroid treatment,
the ulcer had completely healed. This patient subsequently
underwent completion proctectomy with an ileal J-pouch anal
anastomosis (double stapled technique) and a covering loop
ileostomy. The patient is now awaiting ileostomy closure and
is on regular follow up at 2 weekly intervals. Barring an episode
of adhesive intestinal obstruction which was managed
conservatively, the patient is doing well, the steroids have been
tapered, and all operative wounds have healed well with no recurrence of the ulcer.

Case 2
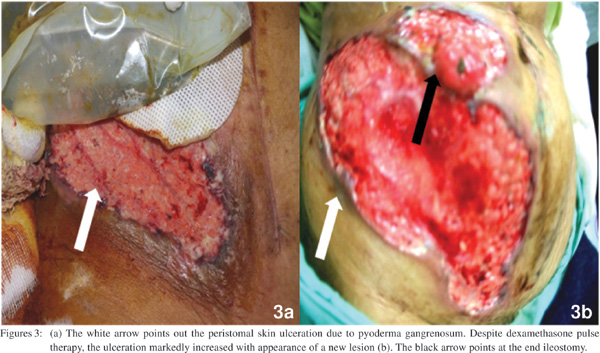
Three months following subtotal colectomy for a severe acute exacerbation of ulcerative colitis (refractory to intensive steroid regimen), a 35-year old lady presented with a painful ulcer (8
cm by 4 cm) around the ileostomy (Figure 3a). She had high grade fever, decreased appetite and complained of increased
rectal bleeding. Proctoscopic examination revealed an inflamed rectal mucosa with ulcerations and pseudopolyps. She had
anemia and a raised erythrocyte sedimentation rate (ESR). A skin biopsy showed features consistent with a diagnosis of
pyoderma gangrenosum. A few days later she developed
another similar lesion on her shin. She was started on
prednisolone (40 mg per day) and received 3 pulses of
dexamethasone (100 mg per day for 5 days every 4 weeks).
Following initial improvement, the peristomal lesion
subsequently worsened with enlargement in size (13 cm by 17
cm) and appearance of a new lesion (Figure 3b). There was
difficulty in applying ileostomy appliance, and the ileostomy
effluent was managed by frequent changes of pads. She also
had persistent rectal bleeding despite being on systemic steroids and topical mesalamine treatment. In view of a relapse
of the pyoderma gangrenosum, and a negligible response to
high dose steroids, she underwent a completion proctectomy
with an ileal J-pouch anal anastomosis (double stapled
technique) and a covering loop ileostomy. Within a month of
the operative procedure, the skin lesions (both peristomal and
shin) healed completely (Figures 4a & 4b). She subsequently
underwent closure of the ileostomy. At the last follow-up, 3
years following her ileostomy closure, the patient was doing
well with good pouch function and no recurrence of the skin
lesions.

Discussion
Peristomal pyoderma gangrenosum (PPG) is a disabling
condition in patients with a stoma. The lesion begins as small
erythematous papules that rapidly spread concentrically, coalesce and subsequently develop central ulceration and
necrosis. The mature lesions have well-defined, undermined,
violaceous border and are very painful.[1]
The exact incidence of PPG is not known. We diagnosed
PPG in 2 of the 250 patients who underwent surgery for
inflammatory bowel disease in our unit. It is possible that the incidence of PPG is higher than reported because PPG is often under-diagnosed or misdiagnosed as stitch abscess, contact
dermatitis, irritation from leaking feces or urine, extension of underlying Crohn’s disease or a wound infection. A high index
of suspicion and familiarity with the appearance of the lesion is needed to make a diagnosis.
The cause of PPG is still debated. The name pyoderma
gangrenosum reflects the historical view of the disease as an
infectious process, but the characteristic lesions are sterile.
Most patients relate the development of the skin lesions to
trauma in the peristomal area. It has been suggested that in
patients with IBD, the development of PPG may reflect the
severity of intestinal disease.[2] The PPG lesions in our first
patient appeared after the withdrawal of steroids. The second
patient had undergone subtotal colectomy for an acute
exacerbation that was refractory to intensive medical
management with steroids. The subsequent appearance and
worsening of pyoderma gangrenosum in this patient, correlated
with worsening of the disease in rectal stump (increased
bleeding per rectum, inflamed rectal mucosa with ulcerations,
anemia and raised ESR).
The time to onset for PPG is variable and may range from a
few months to up to many years. The rapidity of progression is considered to be the hallmark of the disease.[3] Our patients
developed the lesions 3-4 months following creation of the ileostomy and showed rapid progression. The lesions made
stoma care very difficult and labor intensive. In the second
patient, the peristomal lesion was so large that the stomal
appliance could not be applied and the local care of the wound
and stoma was done by frequent change of dressing pads.
The best therapy for PPG is not known. Topical treatment
with steroids, antibiotics or other wound care agents have
been described.[4] However, these modalities may not be suitable
for larger lesions and have no impact on the underlying
intestinal disease.
The other options are to treat the underlying active
inflammation in the gastrointestinal tract. A few reports
describe the use of systemic therapy with high dose steroids,
antibiotics, dapsone, cyclosporine, and infliximab.[5,6,7] Steroid
pulse therapy has also been reported to be effective in some
cases.[8] We managed our first patient with systemic steroids
and he showed a good clinical response. The second patient
was initially managed with prednisolone (40 mg/day) and 3
pulses of dexamethasone pulse therapy (100 mg/day for 5 days
every 4 weeks). However, her skin lesions were refractory to
this treatment. Infliximab was not considered because of its high cost.
The surgical treatment options for PPG include stoma
revision and relocation but these may have failure rates as
high as 40%-100%.[9] Removal of the actively diseased intestinal
segment may be a treatment option in these patients and may
result in healing of the skin lesion.[10] The PPG in our second
patient were refractory to steroids but showed prompt healing
following surgical removal of the diseased rectum.
References
- Callen JP: Pyoderma gangrenosum. Lancet. 1998;351:581–5.
- Hughes AP, Jackson JM, Callen JP: Clinical features and treatment
of peristomal pyoderma gangrenosum. JAMA. 2000;284:1546–8.
- Holt PJ: The current status of pyoderma gangrenosum. Clin Exp
Dermatol. 1979;4:509–16.
- Nybaek H, Olsen AG, Karlsmark T, Jemec GB: Topical therapy for peristomal pyoderma gangrenosum. J Cutan Med Surg.
2004;8:220–3.
- Funayama Y, Kumagai E, Takahashi K, Fukushima K, Sasaki I:
Early diagnosis and early corticosteroid administration improves
healing of peristomal pyoderma gangrenosum in inflammatory
bowel disease. Dis Colon Rectum. 2009;52:311–4.
- Poritz LS, Lebo MA, Bobb AD, Ardell CM, Koltun WA: Management of peristomal pyoderma gangrenosum. J Am Coll
Surg. 2008;206:311–5.
- Sapienza MS, Cohen S, Dimarino AJ: Treatment of pyoderma
gangrenosum with infliximab in Crohn’s disease. Dig Dis Sci.
2004;49:1454–7.
- Galun E, Flugelman MY, Rachmilewitz D: Pyoderma gangrenosum complicating ulcerative colitis: successful treatment with
methylprednisolone pulse therapy and dapsone. Am J
Gastroenterol. 1986;81:988–9.
- Kiran RP, O’Brien-Ermlich B, Achkar JP, Fazio VW, Delaney
CP: Management of peristomal pyoderma gangrenosum. Dis Colon
Rectum. 2005;48:1397–403.
- Talansky AL, Meyers S, Greenstein AJ, Janowitz HD: Does intestinal resection heal the pyoderma gangrenosum of inflammatory bowel disease? J Clin Gastroenterol.
1983; 5:207–10.