|
|
|
|
 |
 |
| |
 |
|
|
Case Report |
|
|
|
|
|
Keywords :
|
|
|
Kirtikumar J offshore Rathod1, Soni Lyndogh1, Ravi Prakash Kanojia1, Kln Rao1
Dept of Pediatric Surgery,1 APC, Block 3-A
Postgraduate Institute of Medical Education and Research,
Sector 12, Chandigarh, India 160012
Corresponding Author:
Dr Ravi Prakash Kanojia
Email: drravikanojia@yahoo.com
DOI:
http://dx.doi.org/
48uep6bbphidvals|423 48uep6bbph|2000F98CTab_Articles|Fulltext Introduction
Hydatid disease (HD) is mostly prevalent in the developing parts of the world.[1] The infestation primarily involves the major visceral organs like the liver, lung and spleen.[2] Disseminated hydatidosis is known to involve the omentum,[3] but primary involvement of the omentum with multiple hydatid cysts is rarely seen.
Case Report
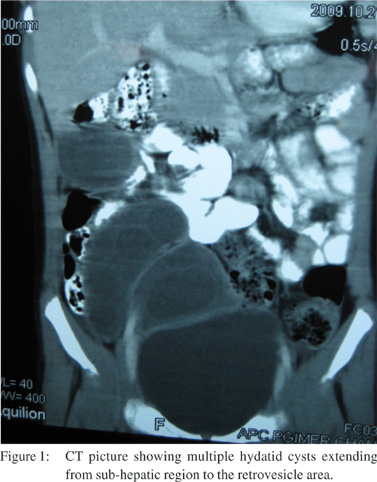
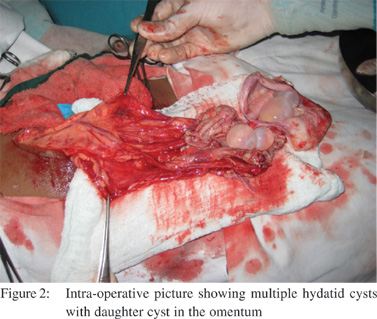
A 12-year-old boy presented to pediatric surgery outpatient department with complaint of abdominal pain for last 3 months. He had also noticed a swelling in the right side of the abdomen since 2 months. There was a vague lump palpable in the right side of the abdomen apparently extending into the pelvis. The lump was non-tender on examination. The ultrasound abdomen clearly showed multiple hydatid cysts with daughter cysts visible inside. This multicystic swelling was extending from the sub- hepatic area adjacent to the gall bladder right up to the retrovesical space. There was no other solid organ involvement present. Hydatid serology was strongly positive. A CECT wasform flimsy adhesions with the surrounding small bowel. The cysts were excised with partial omentectomy and peritoneal toilet was done. There was no other intra abdominal organ involvement. The patient was prescribed another 6 weeks of albendazole treatment. He has completed 9 months of follow up without any complications or recurrence.
Discussion
Hydatid disease is a common entity and typically involves liver or lungs. Atypical involvement of organs like muscles, bones and brain is well described.[4,5] Primary involvement of omentum without disseminated disease is infrequent. Very few cases have been previously described for hydatid disease limited only to omentum in pediatric patients. The mechanism of involvement of these organs is usually secondary to the involvement of liver by escape of daughter micro-cysts in the systemic circulation.[6] Multiple hydatid cysts primarily affecting the omentum without involvement of any other organ is a rare phenomenon. The suggested pathophysiology in this scenario is not very clear. It is described that the hexacanth embryos migrate to liver via portal system. A very few will escape the portal filter and escape to systemic sites like lung via the vena cava and reach lung through right heart circulation, thereby making lung the second commonest site of involvement. Further some oncosphere may escape the lung also and reach the heart again and then spread to the general systemic circulation resulting in various organ involvement.[7] The omentum is rarely affected but can be possibly involved by the above route.
Morris et al[8] have demonstrated that there is a role of enteric lymphatic system also in seeding of oncospheres directly from the gut to the site of development of intra-abdominal cyst. Primary omental hydatids are generally asymptomatic initially. Patients usually present with lump abdomen as an only complaint. On clinical examination this lump can be easily confused with simple omental cyst, mesenteric cyst or enteral duplications cyst. Early diagnosis and treatment is a must, as these cysts can be more prone for complications like torsion, infection and rupture.[9]
The diagnosis of hydatid disease is most of the times straight forward. With the availability of serological tests along with improved imaging modalities early diagnosis can be achieved.[10,11] As described in the present case, ultrasonography easily suggested the abdominal lump to be intra-abdominal hydatid cyst which was confirmed to be arising from the omentum by CT scan. Positive hydatid serology reported in our patient again supplemented our diagnosis.
Although various modalities of treatment like medical management, percutaneous image guided injections of scolicidal agents, open and laparoscopic excision of cyst are described for the treatment of hydatid cyst; only open surgical excision seems to be the appropriate treatment for omental hydatid cyst.[12] This approach can be well justified considering the possibility of torsion, infection, uncontrolled spillage and peritoneal dissemination of the disease by other methods.
Many reports in the literature describe extrahepatic intrabdominal hydatid cysts.[13,14] In a review of similar cases, the reports mentioned in Table 1 describe omental hydatid cysts.[15,16,17,18,19] Out of these 6 reports only 3 reports describe hydatid cyst primarily involving the omentum sparing other organs. It can be seen from the review that with the use of imaging studies diagnosis of the disease is usually easy. A special mention of the report by Thomas in 1877 is an interesting case as it describes a case of 32 yr female with lump in abdomen which the author diagnosed by aspirating the cyst percutaneously and subjecting it to microscopic examination in which he saw hooklets of Echinococcus.[18] As described in our case all the cases of omental hydatid were managed by open surgical cyst excision.
In conclusion, primary omental hydatidosis can occur without any systemic dissemination to other organs. Diagnosis of hydatid cyst should be kept in mind while dealing withchildren with cystic abdominal lump especially in endemic areas. Diagnosis is often easy with present radiologic investigations and serology. Open surgical excision along with medical management should be contemplated to achieve complete clearance thus preventing complications and recurrence.
References
- Lewall DB. Hydatid disease: biology, pathology, imaging and classification. Clin Radiol. 1998;53:863–74.
- Polat P, Kantarci M, Alper F, Suma S, Koruyucu MB, Okur A. Hydatid disease from head to toe. Radiographics. 2003;23:475–94.
- Canda AE. Disseminated hydatid disease. Am J Surg. 2009;198:e3–4.
- Kýresi DA, Karabacakoglu A, Odev K, Karakose S. Uncommon locations of hydatid cysts. Acta Radiol. 2003;44:622–36.
- Bal N, Kocer NE, Arpaci R, Ezer A, Kayaselcuk F. Uncommon locations of hydatid cyst. Saudi Med J. 2008;29:1004–8.
- Molmenti EP, Klein AS. Hepatic infection and acute hepatic failure. In Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Upchurch GR, editors. Greenfield’s Surgery: Scientific principles and practice. 4th ed. Philadelphia: Lippincott Williams& Wilkins; 2006.p.910–24.
- Wani RA, Malik AA, Chowdri NA, Wani KA, Naqash SH. Primary extrahepatic abdominal hydatidosis. Int J Surg. 2005;3:125–7.
- Morris DL, Richards KS. Biology of Echinococcus. Hydatid disease. Current medical and surgical management. Oxford: Butterworth-Heinemann Ltd; 1992.p.7.
- Uramatsu M, Saida Y, Nagao J, Takase M, Sai K, Okumura C, et al. Omental cyst: report of a case. Surg Today. 2001;31:1104–6.
- Liu D, Lightowlers MW, Rickard MD. Evaluation of a monoclonal antibody-based competition ELISA for the diagnosis of human hydatidosis. Parasitology. 1992;104:357–61.
- Yuksel M, Demirpolat G, Sever A, Bakaris S, Bulbuloglu E, Elmas N.. Hydatid disease involving some rare locations in the body: a pictorial essay. Korean J Radiol. 2007;8:531–40.
- Filippou D, Tselepis D, Filippou G, Papadopoulos V. Advances in liver echinococcosis: diagnosis and treatment. Clin Gastroenterol Hepatol. 2007;5:152–9.
- Mosca F, Portale TR, Persi A, Stracqualursi A, Puleo S. Uncommon abdominal sites of hydatid disease. Our experiencewith the surgical treatment of 15 cases. Chir Ital. 2004;56:333–44.
- Daali M, Hssaida R, Zoubir M, Hda A, Hajji A. Peritoneal hydatidosis: a study of 25 cases in Morocco. Sante. 2000;10:255–60.
- Annandale T. Case of large hydatid tumour of the Omentum treated successfully by a free incision, with antiseptic precautions. Br Med J. 1877;27:99.
- Alis H, Kapan S, Öner O, Soylu A, Dolay K, Kalayci MU, Aygun E. Primary omental hydatid cyst. International Medical Case Reports Journal. 2009;1:7–10.
- Sekmenli T, Koplay M, Sezgin A. Isolated omental hydatid cyst: clinical, radiologic, and pathologic findings. J Pediatr Surg. 2009;44:1041–3.
- Durakbasa CU, Tireli GA, Sehiralti V, Sander S, Tosyali AN, Mutus M. An audit on pediatric hydatid disease of uncommon localization: incidence, diagnosis, surgical approach, and outcome. J Pediatr Surg. 2006;41:1457–63.
- Sethi SK, Patnaik S, Narayan, Nayak SN. Isolated omental hydatid cyst—a case report. J Indian Med Assoc. 2004;102:644–6.
|
|
|
 |
|
|