|
|
|
|
 |
 |
| |
 |
|
|
Case Report |
|
|
|
|
|
Keywords :
|
|
|
Rashi Kochha offshorer, Ragesh Babu Thandassery, Birinder Nagi, Rakesh Kochhar
Department of Gastroenterology,
Postgraduate Institute of Medical Education and Research.
Chandigarh-160012, India.
Corresponding Author:
Dr. Rakesh Kochhar
Email: dr_kochhar@hotmail.com
DOI:
http://dx.doi.org/10.7869/tg.2012.114
48uep6bbphidvals|599 48uep6bbph|2000F98CTab_Articles|Fulltext We report a rare case of pancreatic duct–portal vein communication which is not described so far in the literature. The index patient presented with recurrent episodes of abdominal pain and an endoscopic retrograde pancreatography (ERP) incidentally detected communication between the main pancreatic duct and the main portal vein.
Case report
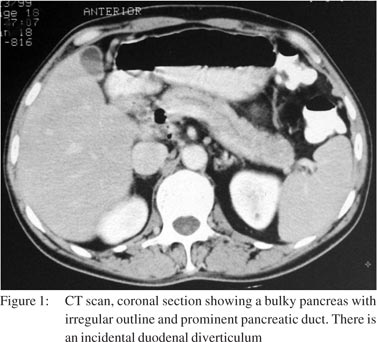
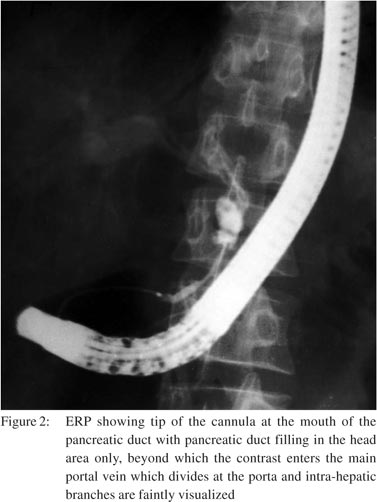
A 42-year-old man was referred to us for recurrent abdominal pain for the past 8 years. The pain was moderate-to-severe, epigastric in location with radiation to the back. It was associated with vomiting occasionally but there was no history of haematemesis or malaena. The last episode of pain was 3 weeks before he presented to us. He had been consuming alcohol, 40–50 g per day for the past 14 years. He did not have any history of endocrine or exocrine pancreatic insufficiency. His physical examination was unremarkable. Investigations showed a normal haemogram and serum biochemistry including blood sugar and serum calcium. Serum amylase was 124 IU/L (normal <70 IU/L). His serum amylase and lipase were always elevated during episodes of pain. A plain X-ray abdomen did not show any calcification. An ultrasound of the abdomen revealed normal pancreatic contour and uneven pancreatic duct with echogenic walls. A contrast-enhanced computed tomography (CECT) scan was done which showed a bulky pancreas with irregular outline and a prominent pancreatic duct; there was in addition evidence of a duodenal diverticulum (Figure 1). The spleno-portal axis was normal. He underwent an ERP using a standard cannula which showed a normal caliber duct in the pancreatic head region which narrowed towards the head–neck junction. The contrast then entered a bulbous vascular channel, which filled the main portal vein, and the intrahepatic branches could be made out (Figure 2). No further injection of contrast was made. The cannula was withdrawn and the papilla observed for any bleeding. The patient did not have any gastrointestinal bleeding or drop in blood pressure. An ultrasound Doppler was done which showed the normal splenic vein and the portal vein. The patient was discharged after 72 hours of observation and started on pancreatic enzyme supplements. He has remained well for the past 4 months.
 Discussion
Our patient had a pancreatic duct–portal vein communication, an occurrence not described previously. Normally, the pancreas is drained by a number of pancreatic veins from the tail, body and head regions which open directly into the splenic vein. The splenic vein joins the superior mesenteric vein to from the main portal vein right behind the neck of the pancreas.[1] The main portal vein then passes upward to the right into the liver hilum. The portal vein is about 8–10 cm long. In our patient, the possible explanations for pancreatic duct–portal vein communication could be either (i) a pancreatic ductal inflammation during the last attack of pancreatitis with a small parenchymal extravasation of contrast which got drained into the main portal vein, or (ii) an aberrant pancreatic vein draining the neck area and opening directly into the main portal vein. The fact that the cannula was only at the mouth of the papillary orifice, much away from the site of pancreatic duct– portal vein communication rules out the possibility of trauma being responsible for the communication. We could not find any similar case in the literature. There are, however, reports of pancreatic pseudocysts communicating with the portal vein.[2,3]
That is attributed to pancreatic enzyme-rich fluid causing disruption of the neighbouring vascular structures. The consequences of pancreatic duct–portal vein fistula can be hemosuccus pancreaticus and portal pyaemia during ERP. Our patient did not have either of the two.
References
Discussion
Our patient had a pancreatic duct–portal vein communication, an occurrence not described previously. Normally, the pancreas is drained by a number of pancreatic veins from the tail, body and head regions which open directly into the splenic vein. The splenic vein joins the superior mesenteric vein to from the main portal vein right behind the neck of the pancreas.[1] The main portal vein then passes upward to the right into the liver hilum. The portal vein is about 8–10 cm long. In our patient, the possible explanations for pancreatic duct–portal vein communication could be either (i) a pancreatic ductal inflammation during the last attack of pancreatitis with a small parenchymal extravasation of contrast which got drained into the main portal vein, or (ii) an aberrant pancreatic vein draining the neck area and opening directly into the main portal vein. The fact that the cannula was only at the mouth of the papillary orifice, much away from the site of pancreatic duct– portal vein communication rules out the possibility of trauma being responsible for the communication. We could not find any similar case in the literature. There are, however, reports of pancreatic pseudocysts communicating with the portal vein.[2,3]
That is attributed to pancreatic enzyme-rich fluid causing disruption of the neighbouring vascular structures. The consequences of pancreatic duct–portal vein fistula can be hemosuccus pancreaticus and portal pyaemia during ERP. Our patient did not have either of the two.
References
- Simeone DM, Mulholland MW. Pancreas: anatomy and structural anamolies. In: Yamada T, Alpers DH, Kaplowitz N, Laine L, Owyang C, Powell DW (eds). Textbook of Gastroenterology, 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2003:2013–26.
- Noh R, Kim HJ. A pancreatic pseudocyst-portal vein fistula closed by endoscopic pancreatic stent insertion. Gastrointest Endosc. 2010;72:1103–5.
- Yoon SE, Lee YH, Yoon KH, Choi CS, Kim HC, Chae KM. Spontaneous pancreatic pseudocyst-portal vein fistula presenting with pancreatic ascites: strength of MR cholangiopancreatography. Br J Radiol. 2008;81:e13–16.
|
|
|
 |
|
|