Eric Wee1, Rajesh Gupta2, Sekaran Anuradha2, Duvuru Nageshwar Reddy2, Sundeep Lakhtakia2
Khoo Teck Puat Hospital1, Singapore.
Asian Institute of Gastroenterology2,
Hyderabad, India
Corresponding Author:
Dr. Eric Wee
Email: wee1976@gmail.com
DOI:
http://dx.doi.org/10.7869/tg.285
48uep6bbphidvals|1349 48uep6bbphidcol2|ID 48uep6bbph|2000F98CTab_Articles|Fulltext A proportion of patients will have no identifiable cause of their chronic pancreatitis and are diagnosed with idiopathic chronic pancreatitis. In this report, we discuss a case of primary hyperparathyroidism presenting as chronic pancreatitis to the gastroenterologist.
Case report
A 27-year-old male was referred to a tertiary gastrointestinal hospital for the complaint of recurrent epigastric pain of 4 months duration. He had been evaluated at another hospital and was diagnosed with chronic pancreatitis based on a CT scan. He had elevated serum amylase and lipase at the time of initial presentation. The cause of his chronic pancreatitis was presumed idiopathic, as he was a teetotaller and did not have gallstones or hypertriglyceridemia.
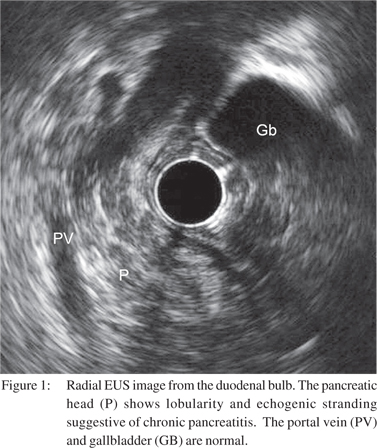
We evaluated the pancreas and biliary tree with endoscopic ultrasound. A radial echoendoscope (GF-UE160, Olympus Optical Co, Ltd, Tokyo, Japan) was inserted with the patient under moderate sedation. The pancreas showed diffuse hyperechoic strands, echogenic foci, honeycombing and lobularity (Figure 1). The pancreatic duct was irregular, but not dilated. There were no pancreatic ductal stones or pseudocysts. The stack sign was observed from the duodenal bulb, suggesting that pancreas divisum was unlikely. Examination of the biliary tree and gallbladder did not reveal any microlithiasis. These features were consistent with a diagnosis of chronic pancreatitis.
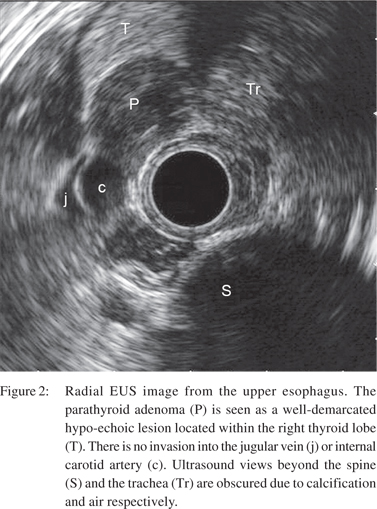
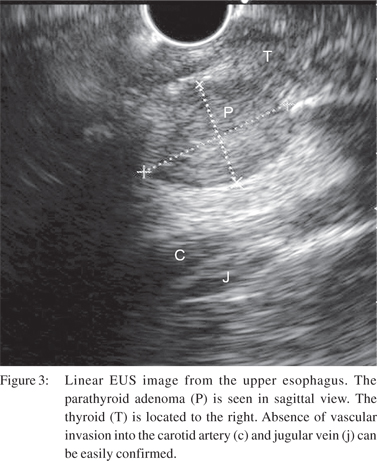
Upon withdrawal of the echoendoscope, a wellcircumscribed, homogeneous, hypo-echoic mass with distinct margins was visualised from the proximal oesophagus. The lesion was identified as arising from within the right lobe of the thyroid gland. It measured 21 mm by 14 mm in diameter (Figure 2). This lesion was further investigated with a linear echoendoscope (GF-UCT180, Olympus Optical Co, Ltd, Tokyo, Japan). There were no features of vascular invasion or mediastinal lymphadenopathy (Figure 3).
The lesion was suspected to be either a parathyroid or thyroid tumour. His serum calcium levels were marginally elevated at 12.8 mg/dL (normal 8-10 mg/L). In addition, his parathyroid hormone levels were elevated at 207.5 pg/mL (normal 10-55 pg/ml). A technetium-99m sestamibi scintigraphy scan confirmed the EUS diagnosis of a parathyroid tumour.
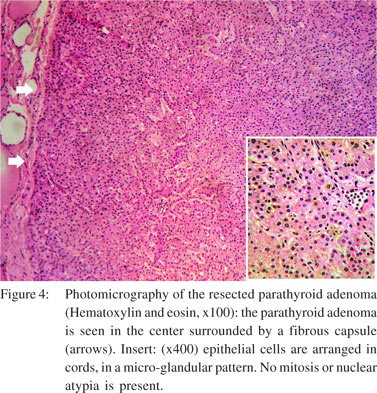
The patient underwent surgical excision of the lesion. The specimen was confirmed on histology to be a parathyroid adenoma (Figure 4). Post-resection, his calcium levels normalised. Further evaluation for tumours associated with the multiple endocrine neoplasia (MEN) syndrome was negative. The etiology of his chronic pancreatitis was due to hypercalcaemia from a parathyroid adenoma.
Discussion
Primary hyperparathyroidism and hypercalcaemia may present with gastrointestinal problems such as constipation, anorexia, nausea and abdominal pain. Hyperparathyroidism has also been associated with acute and chronic pancreatitis. Despite numerous reports of patients with both pancreatitis and primary hyperparathyroidism, the association between these 2 diseases still remains somewhat controversial. This is due to the fact that not all patients with primary hyperparathyroidism will develop pancreatitis. The incidence of acute pancreatitis in patients with primary hyperparathyroidism has been reported to be between 1.5% and 12% only.[1-3] One large retrospective analysis revealed that primary hyperparathyroidism was associated with a 28-fold increased risk of developing pancreatitis as compared to patients without hyperparathyroidism.[4] Examination of the parathyroid and thyroid glands are not part of the routine EUS evaluation. However, a parathyroid tumour may be detected at EUS and this has been described in a case series by Catargi B et al.[5] Typical imaging characteristics of a parathyroid adenoma on ultrasound are a hypo-echoic structure, with regular borders and homogeneous echotexture. Features suggestive of a carcinoma based transcutaneous ultrasound images are an enlarged lesion with irregular borders, and a heterogeneous echotexture. In normal patients, the parathyroids are usually not visualised.
The sensitivity of EUS as compared to transcutaneous ultrasound and scintigraphy scan is inadequately studied. Neither has the learning curve to achieve competency and the inter-operator variability been evaluated. Therefore, EUS cannot substitute existing imaging modalities as a screening tool if a patient is suspected to have a parathyroid adenoma.
References
- Cope O, Culver PJ, Mixter CG Jr, Nardi GL. Pancreatitis, a diagnostic clue to hyperparathyroidism. Ann Surg. 1957;145:857–63.
- Bess MA, Edis AJ, van Heerden JA. Hyperparathyroidism and pancreatitis. Chance or a causal association? JAMA. 1980;243:246–7.
- Jacob JJ, John M, Thomas N, Chacko A, Cherian R, Selvan B, et al. Does hyperparathyroidism cause pancreatitis? A South Indian experience and a review of published work. ANZ J Surg. 2006;76:740–4.
- Ward JB, Petersen OH, Jenkins SA, Sutton R. Is an elevated concentration of acinar cytosolic free ionised calcium the trigger for acute pancreatitis? Lancet. 1995;346:1016–9.
- Catargi B, Raymond JM, Lafarge-Gense V, Leccia F, Roger P, Tabarin A. Localization of parathyroid tumors using endoscopic ultrasonography in primary hyperparathyroidism. J Endocrinol Invest. 1999;22:688–92.
|