48uep6bbphidcol2|ID
48uep6bbphidvals|1936
48uep6bbph|2000F98CTab_Articles|Fulltext
Celiac disease (CD) is a chronic small-intestinal immune-mediated enteropathy precipitated by exposure to dietary gluten in genetically predisposed individuals. CD patients often present with diarrhea, steatorrhea, abdominal discomfort, bloating, flatulence, anemia and/or weight loss. It is not infrequent to diagnose gastrointestinal motor abnormalities in celiac patients. Untreated celiacs may exhibit disturbed esophageal motility, altered gastric emptying, and dysmotility of the small intestine, gallbladder and colon.1 However, dysphagia has never been considered as a major symptom in CD patients, and most of the publications on gastro-intestinal symptoms of CD do not mention dysphagia.2 Also, CD is rarely considered in the differential diagnosis of a patient presenting with motor dysphagia. Suspecting and treating CD in patients with dysphagia is important as this leads to almost complete resolution of symptomsand is very rewarding for the patient. We report a case of a middle age female presenting with dysphagia, who was diagnosed to have celiac disease with esophageal motor abnormalities.
Case Report
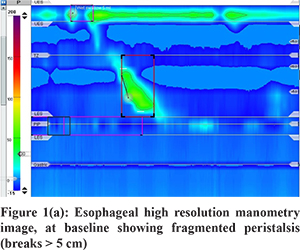
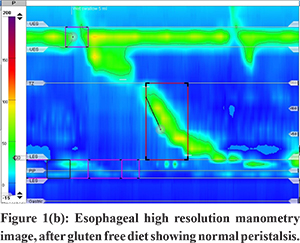
A 55-year-old female presented with history of progressive dysphagia to both solids and liquidsfor one year, associated with weight loss of approximately 20% of her body weight. General physical examination revealeda low body mass index (20 kg/m2) and pallor. Investigations revealed haemoglobin of 9.0 gm/dL and ferritin of 6.0 ng/mL. Liver function tests, renal function tests, bloodsugar and thyroid function testswere normal. Esophagogastroduodenoscopy was performed for evaluation of dysphagia, which revealed significant scalloping of the duodenal folds. Duodenum biopsy was suggestive of Marsh III villous atrophy and esophageal biopsies showed no evidence of eosinophilic esophagitis. Subsequently, serum anti-tissue transglutaminase antibody testing was done, which reported levels of >300 U/ml. High resolution esophageal manometry revealed fragmented peristalsis (esophageal peristaltic breaks of>5 cm in 80% of the contractions) with normal lower esophageal sphincter (LES) pressure and normal IRP4 (integrated relaxation pressure 4 seconds) (Figure 1(a)). The patient was started on a gluten free diet and oral iron supplements. The patient showed symptomatic improvement with resolution of dysphagia, increase in weight and haemoglobin within 4 weeks. Repeat high resolution manometry after 4 months showed significant improvement in esophageal peristaltic activity(no peristaltic contraction having breaks to > 5 cm) (Figure 1(b)).
Discussion
Celiac disease has been associated with multiple gastrointestinal motor abnormalities withdyspahgia being one of them. Current data shows the presence of disturbed motility of the oesophagus, stomach and colon in untreated celiac disease.1 There are several hypotheses that may explain gastrointestinal motility disorders in patients with celiac disease. It has been hypothesised that the intense mucosal damage observed in celiac disease may alter the contractile upper-gut activity through perturbations of the complex hormonal and neuro- immunomodulatory regulation in the intestinal mucosa.
Hormonal derrangements play a key role in the motility disorders of celiac diseasesince the secretion of several hormones is altered in celiac disease as a consequence of intestinal mucosal damage. Inflammatory mediators and neurotransmitters are released at the gut wall. The bowel becomes hypersensitive to physiologic stimuli which may explain the sensorimotor abnormalities. Postprandial cholecystokinin (CCK) levels are low in untreated celiac patients despite the concomitant increase in the number of duodenal CCK secreting cells. Neurotensin (NT), a peptide released from the distal ileum, is capable of inhibiting upper gastrointestinal motility and gastric emptying. Increased serum NT levels has been found in untreated CD. Basal plasma peptide YY level in untreated CD are elevated, which may inhibit gastrointestinal motility and decrease LES pressure. Somatostatin levels are increased in untreated celiac disease and associated with reduced gastric motility. The motility defectsin the gall bladder and the small intestine in celiac disease are mainly caused by reduced cell secretion following meals. The clinical consequence of these alterations is that the esophageal transit, gastric and gall bladder emptying and orocaecal transit are delayed while colonic transit is faster. Delayed gastric emptying and slower orocoecal peristalsis time can also be explained by abnormal exposure of the small bowel to unabsorbed fat, which is proportional to the length of the bowel exposed to this nutrient.
An immune disorder is another important mechanism in celiac disease and inflammation that may by itself produce a marked motility disorder. It is hypothesised that an extrinsic autonomic neuropathy, although subclinical, could disarrange uppergut motor function in celiac disease. Usai et al studied the autonomic nervous system in 36 untreated adult celiac patients withesophageal manometry and pH metry. They demonstrated that celiac patients showed autonomic dysfunction, which correlated significantly with the age, percentage of esophageal bi-peaked waves, and the number of intestinal fasting clusters.3 In another study, the same author studied 36 patients with celiac disease for the presence of osephageal motility abnormalities. Fifty percent of the patients complained of dysphagia. Manometric evaluation was done in 18 subjects and 67% patients showed motor abnormalities consisting of nutcracker esophagus, hypotonic lower esophageal sphincter and frequent repetitive (>3 peaks) contractions.4
In another study, Iovino P et al studied 22 adult celiac patients, with and without steatorrhea. Before starting a gluten-free diet, the prevalence of esophageal symptoms was 45.5% in all patients, but they were significantly higher in patients with steatorrhea. Also, the lower oesophageal sphincter pressure was 17.5+/-5.3 in all patients, but was significantly lower in patients with steatorrhea. They observed that after the introduction of a gluten free diet, the prevalence of esophageal symptoms diminished (9% vs 45.4%, p < 0.05) and the lower oesophageal sphincter pressure increased.5
This is the first case report from our region, which demonstrates esophageal motility abnormalities by high resolution esophageal manometry in a patient of CD presenting with dysphagia and also describing the reversal of theseabnormalities with a gluten free diet. Thus, we highlight the fact that CD should be kept as a differential diagnosis in patients presenting with motor dysphagia, even in the absence of typical celiac symptoms, especially in high prevalence regions.
References
- Tursi A. Gastrointestinal Motility disturbances in celiac disease. J Clin Gastroenterol. 2004; 38:642-45.
- Spijkerman M, Tan IL, Kolkman JJ,Withoff S, Wijmenga C, Visschedijk MC, et al. A large variety of clinical features and concomitant disorders in celiac disease - A cohort study in the Netherlands. Dig Liver Dis. 2016;48(5):499-505.
- Usai P, Usai Satta P, Lai M,Arciprete F, Brandimarte G, Capria A, et al. Autonomic dysfunction and upper digestive functional disorders in untreated adult celiac disease. Eur J Clin Invest. 1997; 27:1009–15.
- Usai P, Bassotti G, Usai Satta P, Cherchi M, Plesa A, Boy F, ,et al. Oesophageal motility in adult coeliac disease. Neurogastroenterol Mot. 1995;7:239-244.
- Iovino P, Ciacci C, Sabbatini F, Acioli DM, D’Argenio G, Mazzacca G. Esophageal impairment in adult celiac disease with steatorrhea. Am J Gastroenterol. 1998;93:1243–9.