Sarcoidosis is a systemic granulomatous disease characterized by the formation of non caseating epithelioid granulomas. Lung is the most common organ involved in sarcoidosis. Liver involvement in sarcoidosis as initial presentation is uncommon and symptomatic hepatic sarcoidosis occurs in less than 5 to 15 percent.1 Most patients are asymptomatic and have only biochemical abnormalities. Clinically apparent liver disease is uncommon even in patients who have numerous hepatic granulomas in the absence of respiratory symptoms. Rarely patients develop cholestatic liver disease, cirrhosis, portal hypertension, and/or hepatic vein thrombosis. Thus, the additional steps of identifying characteristic extrahepatic manifestations of sarcoidosis (e.g. cutaneous manifestations and/or chest X-ray abnormalities), and ruling out other possible causes such as infection (particularly mycobacterial and fungal), drug-induced granulomas, and malignancy, are essential to make a definitive diagnosis. The treatment of hepatic sarcoidosis depends upon the clinical manifestations of the disease.
Here, we present a case series of three patients who presented with liver disease as the first presentation of sarcoidosis.
Case 1
A 53-year-old man, a known case of diabetes mellitus presented with complaints of significant weight loss and fatigue since 6 months. Before 6 months, he was evaluated in a private hospital and a diagnosis of hepatobiliary tuberculosis was made. Subsequently, he was started on antitubercular drugs and even after 6 months of ATT, the patient did not improve clinically. On evaluation, he had hepatosplenomegaly with normal respiratory, cardiovascular and nervous systems examination.
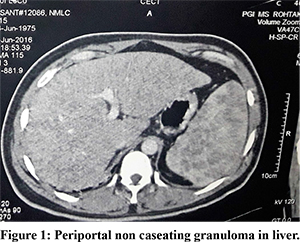
Laboratory investigations revealed anemia with haemoglobin of 7.8 g/dL. He had elevated serum alkaline phosphatase (SAP) 1252 U/L, serum bilirubin 2.9 mg/dl with normal aspartate aminotransferase (AST) and alanine aminotransferase (ALT) values suggestive of cholestatic pattern. Renal functions tests were deranged with blood urea 136 mg/dl and serum creatinine 3.1 mg/dl. Serum calcium and serum 1,25 dihydroxyvitamin D levels were elevated to 13 mg/dl (8.5-10.5 mg/dL) and 256 pmol/L, respectively. Serum angiotensin converting enzyme (ACE) levels were increased with values of 112U/L(normal <60). Mantoux test was negative. Percutaneous liver biopsy revealed the presence of non caseating periportal granulomas (Figure 1). Chest X-ray was within normal limits, but pulmonary function tests showed a restrictive pattern. CECT Chest showed subpleural, interlobular and interlobular interstitial thickening in bilateral lower lobes and posterior segment of both upper lobes along with subcentimetric lymph nodes suggestive of interstitial lung disease. Presence of noncaseating liver granulomas, interstitial lung disease and increased serum ACE levels lead to diagnosis of hepatic sarcoidosis. Patient was started on steroids with insulin for diabetes leading on to improvement in clinical symptoms and biochemical parameters. Adequate hydration improved hypercalcemia and renal dysfunction. Later patient developed hoarseness of voice. Evaluation revealed vocal cord nodules on laryngoscopy examination. Therefore, sarcoidosis had involved liver, lung and vocal cords and it showed response to steroids.
Case 2
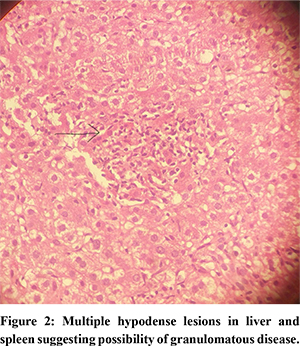
A 41-year old diabetic male was referred with a diagnosis of cirrhosis of liver to hepatobiliary clinic. Patient revealed history of fatigue and weight loss since last 6 months. There was no history of dyspnea, cough or expectoration. On examination, hepatomegaly was present with a firm nodular surface and there was no ascites. Etiological evaluation revealed cholestatic pattern of LFTs with raised SAP levels and normal transaminases. Viral and autoimmune markers was non-contributory. Magnetic resonance cholangiopancreatography revealed no evidence of biliary obstruction. Triple phase CECT whole abdomen showed enlarged liver with multiple scattered ill-defined, ill marginated hypodense areas and mildly enlarged spleen with ill defined hypotense areas suggestive of a granulomatous disease. A possibility of infiltrative liver disease was kept. Serum ACE levels were raised with normal kidney function test and calcium levels. Chest X-ray was within normal limits. CECT chest showed multiple lymph nodes in pretracheal, subcarinal andhilar region with patchy areas of consolidation in right middle and left lower lobe of lung (Figure 2). Transbronchial lung biopsy showed presence of scattered non caseating epitheliod cell granulomas suggestive of sarcoidosis. A diagnosis of sarcoidosis with liver and lung involvement was kept and patient was started on steroids.
Case 3
Third patient was a 60-year old male was referred to hepatobiliary clinic for evaluation of cirrhosis. On physical examination hepatosplenomegaly was present. Respiratory and cardiovascular systems were unremarkable. Investigations revealed cholestatic pattern with raised SAP levels and normal transaminases. Viral and autoimmune markers was non contributory.Hypercalcaemia was present with raised serum ACE levels. CECT chest and abdomen revealed multiple nodules predominantly in peribronchial location with enlarged bilateral hilar and mediastinal lymph nodes and hepatosplenomegaly suggestive of a granulomatous disease. PET-CT was done showing metabolic active cervical, mediastinal and abdominal lymphadenopathy with metabolic active miliary hypodensities in liver and spleen. Transbronchial lung biopsy revealed non caseating granulomas suggestive of sarcoidosis. Patient has been started on steroids and has improved symptomatically.
Discussion
Although liver involvement as a presenting manifestation is uncommon in sarcoidosis, it rarely causes symptoms and may remain undiagnosed in many cases. The clinical consequences of the involvement are variable.2 Hepatic sarcoidosis is approximately twice as common in African-Americans as Caucasians. The clinical consequences of liver involvement are variable and can cause cholestatic jaundice, portal hypertension, cirrhosis and can lead to end stage liver disease. Most patients with hepatic sarcoidosis are asymptomatic and have only biochemical abnormalities like raised alkaline phosphatase levels. Abdominal pain and pruritus are noted in approximately 15 percent of affected patients, and hepatomegaly in 5 to 15 percent of patients.3 Fever, weight loss, and jaundice are present in less than 5 percent of patients.3 Rarely patients develop cirrhosis, cholestatic liver disease with diffuse intrahepatic biliary strictures resembling sclerosing cholangitis, obstructive jaundice due to periportal lymphadenpathy or hepatic vein thrombosis. Portal hypertension may develop as a result of biliary fibrosis or cirrhosis, or rarely due to periportal granulomas that restrict portal flow. Thrombosis of hepatic vein may be related to either external compression by granuloma or direct granulomatous involvement of the hepatic vein resulting in luminal narrowing and stasis.4 Abnormal liver function tests are encountered in 20-40% and usually reveal a cholestatic pattern.5 Increased alkaline phosphatase, gamma glutamyl transpeptidase, bilirubin (usually <5mg/L) and slightly elevated aminotransferase levels are typical laboratory findings.5 Contributing factors for cholestasis seems to be the progressive interlobular bile duct injury due to inflammatory infiltration of basement membranes and portal granuloma formation. Hypoalbuminemia is rare and can be a manifestation of cirrhosis. Other biochemical abnormalities include raised calcium levels and raised serum ACE levels due to increased 1,25 dihydroxyvitamin D activity in granuloma cells.6
Asymptomatic hepatic lesions may be first identified on computed tomography (CT) as hepatomegaly with numerous hypodense nodular lesions7 Magnetic resonance imaging shows hypointense nodular lesions on T1-weighted images, while hyperintense nodules relative to the surrounding liver parenchyma on T2-weighted images.8
Liver biopsy is usually recommended for diagnosis. Typically, the majority of biopsy specimens greater than 2 cm in length will have noncaseating granulomas that are often located along the portal tract. As conditions other than sarcoidosis can cause granulomatous lesions in the liver (e.g. tuberculosis, fungal infections, brucellosis, Q fever, primary biliary cholangitis, Hodgkin disease, drug toxicity etc.), additional features are needed to make a definite diagnosis of sarcoidosis. These features include identifying characteristic extrahepatic manifestations of sarcoidosis (cutaneous manifestations and/or chest imaging abnormalities), characterization of the granulomas within the liver (location and appearance), examination of special stains/cultures for infectious organisms, and exclusion of malignancy and drug-induced granulomas.
FDG-PET/CT technique is emerging as diagnostic tool in the staging and identification of occult sites, sites suitable for biopsy and for the assessment of active sarcoidosis in patients with prolonged symptoms, especially when other markers of the disease are within normal limits. FDG accumulates in activated inflammatory cells and simultaneously provide PET and CT images. FDG-PET/CT also provides a better visualization of extrathoracic sites of active sarcoidosis, such as in the bones, liver, spleen, and retroperitoneal lymph nodes. FDG-PET/CT also has a role in the clinical management of patients with chronic persistent sarcoidosis, such as for planning treatment, monitoring response, and long-term follow-up.
Establishing a definitive diagnosis of hepatic sarcoidosis depends on three components:
* Biopsy evidence of noncaseating granulomas in the “symptomatic or incident organ”
* Exclusion of other causes of granulomatous disease, particularly mycobacterial, fungal, and parasitic infections
* Clinical, radiographic, and optimally histopathologic evidence of sarcoidosis in at least one other organ system
In our case series, all 3 patients had a histological evidence of sarcoidosis through biopsy and involvement of liver and lung.
Evidence based guidelines for the treatment of hepatic sarcoidosis are lacking. Patients with severe symptoms and extrahepatic organ involvement require treatment. Controversy arises when hepatic sarcoidosis is asymptomatic and the main presenting feature, while extra-hepatic involvement is not life threatening and doesn’t require treatment. Generally, the clinical course for sarcoidosis varies. Independently of the localization, in half of cases, disease resolves spontaneously within 2 years.9 Regarding liver sarcoidosis, although corticosteroids may improve clinical and laboratory parameters, however reversal of histological changes is not fully acheived. In our series, all the three patients are treated with corticosteroids and have improved symptomatically. In a retrospective cohort of 17 patients, UDCA at a dose of 13-15 mg/kg daily had a positive effect on pruritus and liver biochemistry, supporting the empirical use of UDCA in the treatment of hepatic sarcoidosis.10 In case of end stage liver disease with complications of portal hypertension, some patients may need liver transplantation.11
References
- Judson MA. Extra pulmonary sarcoidosis. Semin Respir Crit Care Med 2007; 28(1):83-101
- Tan CB, Rashid S, Rajan D, et al. Hepatic sarcoidosis presenting as portal hypertension and liver cirrhosis: case report and review of the literature. Case Rep Gastroenterol 2012; 6:183-89.
- Devaney K, Goodman ZD, Epstein MS, et al. Hepatic sarcoidosis. Clinicopathologic features in 100 patients. Am J SurgPathol 1993; 17:1272-80
- Efe C, Shorbagi A, Ozseker B, Yimaz H, Sokmensuer C, Ferhun B et al. Budd-Chiari syndrome as a rare complication of sarcoidosis. Rheumatol Int. 2012 Oct;32(10):3319-20.
- Karagiannidis A, Karavalaki M, Koulaouzidis A. Hepatic sarcoidosis. Ann Hepatol. 2006 Oct-Dec;5(4):251-6.
- Studdy PR, Bird R. Serum angiotensin converting enzyme in sarcoidosis--its value in present clinical practice. Ann ClinBiochem 1989; 26 (1):13-8.
- Scott GC, Berman JM, Higgins JL Jr. CT patterns of nodular hepatic and splenic sarcoidosis: a review of the literature. J Comput Assist Tomogr 1997; 21:369-72.
- Jung G, Brill N, Poll LW, et al. MRI of hepatic sarcoidosis: large confluent lesions mimicking malignancy. AJR Am J Roentgenol 2004; 183:171-3.
- Valeyre D, Prasse A, Nunes H, Uzunhan Y, Brillet PY, Müller-Quernheim J. Sarcoidosis. Lancet. 2014 Mar 29;383(9923):1155-67.
- Bakker GJ, Haan YCL, Maillette de Buy Wenniger LJ, Beuers U. Sarcoidosis of the liver: to treat or not to treat? Neth J Med. 2012 Oct;70(8):349-56.
- Tombazzi C, Waters B, Ismail MK, Sylvestre PB, Martinez-Hernandez A, Riely CA. Sarcoidosis mimicking primary sclerosing cholangitis requiring liver transplantation. Ann Hepatol. 2008 Jan-Mar;7(1):83-6.