Neuroendocrine tumors (NETs) are a type of heterogeneous tumors that develop from neuroendocrine cells and Kulchitsky cells that can release neurotransmitter peptides. It was first described by Oberndorfer in 19071. Gastrointestinal tract (73.7%) followed by the respiratory system (21%) are the most common sites for NETs. NETs can be found in any location of the body; however, as mentioned above, they are commonly seen to involve gastrointestinal and pulmonary systems2. Gall bladder neuroendocrine tumors (GB-NETs) are extremely rare, accounting for approximately 0.2% of all NETs and 2% of all gall bladder carcinomas3.
Case Report
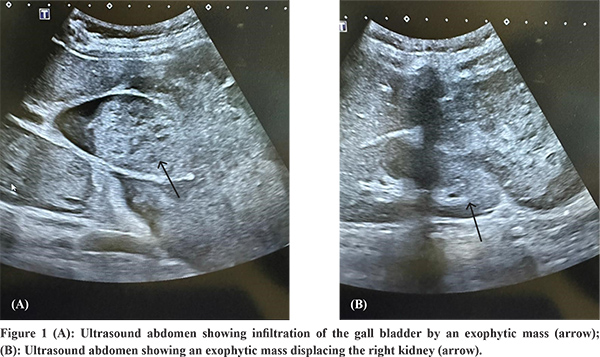
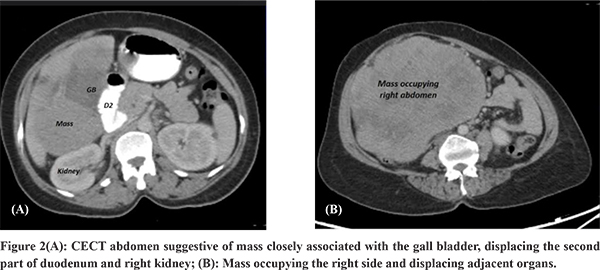
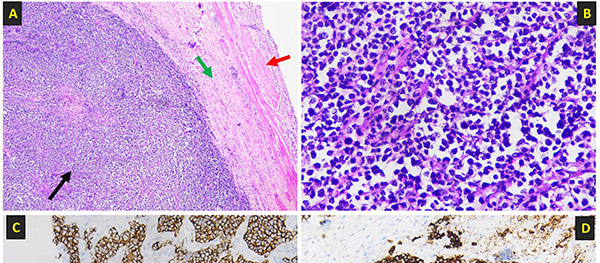
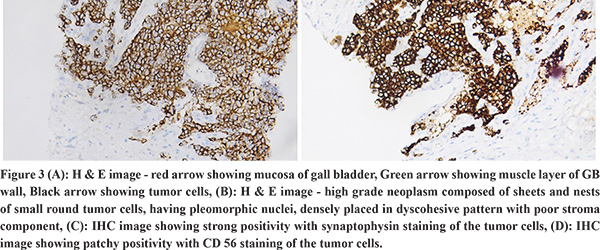
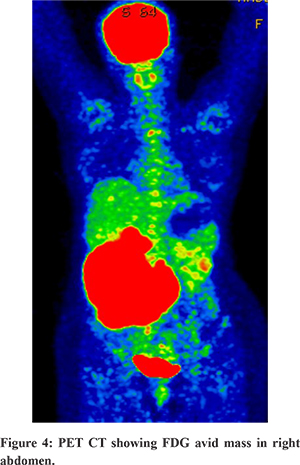
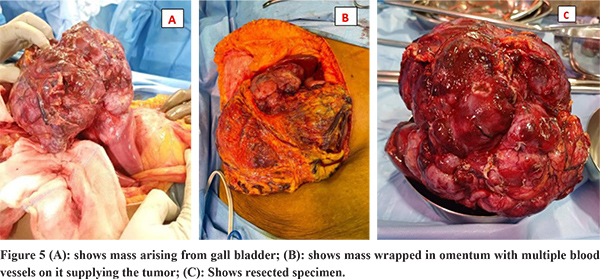
We present a case of a well preserved (WHO performance status 1) 42-year-old lady, without co-morbidities,who came to us with complaints of a lump in the right side of her abdomen and abdominal pain for 4 months. To start with, the lump was small and had gradually progressed over 4 months to occupy the entire right side of the abdomen. This was associated with a non-radiating, dull-aching abdominal pain in the right hypochondrium, which was not associated with meals, nausea, vomiting, hematemesis, jaundice, fever or altered bowel habits. She had loss of appetite and weight loss of approximately 6 kilograms since then. On physical examination, she was pale, and a large tender hard mass, approximately 20 cm in size was palpable, occupying the right hypochondrium, epigastrium, and right lumbar region. Laboratory investigations revealed anemia, liver, and renal biochemistry were within normal limits. CA 19-9 was within normal limits. She underwent ultrasonography (USG) of the abdomen, which was suggestive of a hyperechoic exophytic right hepatic mass lesion of size approximately 20 cm involving the gall bladder wall and extending into the right paracolic gutter compressing and displacing the right kidney and adrenals (Figure 1A and 1B). CT abdomen was suggestive of a mass closely associated with the gall bladder, displacing the second part of duodenum and right kidney (Figure 2A). Figure 2B is suggestive of a mass occupying the right side of abdomen and displacing adjacent organs. In view of locally advanced disease, patient underwent USG guided biopsy of the mass. Histopathological examination (HPE) was suggestive of an infiltrating neoplasm composed of irregular nest of cells with pleomorphic hyperchromatic nuclei and scant cytoplasm. Immunohistochemistry (IHC) was positive for Synaptophysin, EMA, CD56, NKX2.2, and Desmin. Ki 67 index was 2-3 mitoses/hpf (Figure 3A-D). HPE with IHC was suggestive of poorly differentiated NET- Grade 3. PET CT was done which was suggestive of a large lobulated heterogeneously enhancing metabolically active mass in subhepatic region probably arising from the gall bladder causing subtotal luminal obliteration with the lesion indenting adjoining hepatic parenchyma (Segment 4B, 5 and 6), anteriorly the lesion extended upto the anterior abdominal wall, posteriorly it compressed the hepatic flexure and proximal transverse colon, and also indented the anterior cortex of right kidney. There was loss of fat plane between the lesion and proximal duodenum- suspicious of infiltration and metabolically active enlarged periportal/portocaval nodes were present (Figure 4). PET-CT findings were suggestive of a primary gall bladder malignancy with lymphnode spread and no obvious distant metastases. After discussion with multi-disciplinary team (MDT), the patient underwent staging laparoscopy which showed no hepatic or peritoneal metastases, and hence we proceeded to open radical cholecystectomy. The intra operative findings were as follows: approximately 20 x 18 cm tumor arising from gall bladder was seen which was receiving significant blood supply from omentum. Few enlarged periportal lymph nodes were present. 17 lymphnodes were removed. “No other structures were involved” and the resected specimen was sent for HPE which was suggestive of poorly differentiated small round cell neoplasm with mitotic rate of 2-3/hpf, 7 of the 17 nodes were positive for metastases and a pathological stage of pT3N2 was given (Figure 5A-C). The patient recovered well post-surgery and subsequently a medical oncologist opinion was taken and the patient was advised for adjuvant chemotherapy.
Discussion
Gall bladder is a rare site for neuroendocrine cells. The etiology for Gall bladder NET is uncertain. Few suggestions have been proposed to explain its etiology. First, intestinal metaplasia produced by long-term inflammation of the gall bladder mucosa is the cause. Secondly, undifferentiated gall bladder stem cells have the capacity to differentiate into neuroendocrine cells, which is where GB-NET can originate. Third, it can be seen in adenocarcinoma differentiation resulting from metaplasia or trans-differentiation. Fourth, NET can develop from heterotopic pancreatic tissue in the gall bladder4. Most of the patients with GB-NET have a non-specific presentation and can present with abdominal pain, weight loss and jaundice since most of them are non-functional5. Only a few cases of functional GB-NET have been reported who have specific clinical features related to neuropeptides released4. Our patient was of the non-functional type who did not have features related to secreted neuropeptides.
Abdominal ultrasonography, contrast-enhanced CT, and MRI/MRCP do not reveal any specific diagnostic signs. However, these studies are helpful for staging and managing the disease. In terms of imaging, GB adenocarcinoma is the most common differential with other GB malignancies. NETs are hypervascular tumors. They are hyperenhancing on the arterial phase6. Lymph nodes (88%), liver (88%), lung (23%), and peritoneum (19%) are the most common site for metastases7. This was consistent with our case. Usually patients are diagnosed in an advanced stage when there is invasion of the hepatic parenchyma or lymphovascular invasion has already occurred leading to poor prognosis2. FDG PET has a limited role in NET as majority of them are metabolically inactive and do not take up 18- fluorodeoxyglucose (FDG). However avid uptake of 18-FDG has been seen in poorly differentiated NET which are aggressive in nature6. Similar finding was seen in our case.
HPE and IHC are of utmost importance for diagnosis. Currently available biomarkers are synaptophysin, chromogranin A and neuron-specific enolase (NSE)2.
Treatment ranges from simple cholecystectomy to extensive radical resection. Platinum based chemotherapy with Etoposide has shown benefit3. Symptoms of carcinoid syndrome can be managed with somatostatin analogues4. Neoadjuvant protocols have not been established in view of rarity and there is no standardized established treatment modality.
Conclusion
GB-NET is a rare entity. Owing to its rarity, there is limited literature available. GB-NET should also be kept in differential diagnosis in a patient who has a Gall bladder mass. Currently there are no standard treatment protocols available. Early diagnosis and surgical intervention may give the patient a better outcome.
Highlights
• GB-NET is an extremely rare disease accounting for approximately 0.2% of all NETs
• Large tumor size without evidence of systemic metastases
• The patient was well preserved despite having such a large tumor
• The lesion was deemed resectable on staging laparoscopy
References
- Modlin IM, Lye KD, Kidd M. A 5-decade analysis of 13,715 carcinoid tumors. Cancer. 2003 Feb 15;97(4):934–59.
- Kumar K, Tariq H, Ahmed R, Chukwunonso C, Niazi M, Ihimoyan A. Small-Cell Type, Poorly Differentiated Neuroendocrine Carcinoma of the Gallbladder: A Case Report and Review of the Literature. Case Rep Oncol Med. 2019 Apr 1;2019:e8968034.
- Yao JC, Hassan M, Phan A, Dagohoy C, Leary C, Mares JE, et al. One hundred years after “carcinoid”: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol. 2008 Jun 20;26(18):3063–72.
- Marak JR, Kumar T, Dwivedi S, Khurana R. Neuroendocrine tumor of the gall bladder: A rare case report with review of literature. Radiol Case Rep. 2023 Aug 26;18(11):3912–6.
- Shimizu T, Tajiri T, Akimaru K, Arima Y, Yoshida H, Yokomuro S, et al. Combined neuroendocrine cell carcinoma and adenocarcinoma of the gallbladder: report of a case. J Nippon Med Sch Nippon Ika Daigaku Zasshi. 2006 Apr;73(2):101–5.
- Maxwell JE, Howe JR. Imaging in neuroendocrine tumors: an update for the clinician. Int J Endocr Oncol. 2015;2(2):159–68.
- Yun SP, Shin N, Seo HI. Clinical outcomes of small cell neuroendocrine carcinoma and adenocarcinoma of the gallbladder. World J Gastroenterol. 2015 Jan 7;21(1):269-75.