Rajni Yadav, Saumyaranjan Mallick, Deepak Mittal1, Madhusudhan KS2, Manisha Jana2, Minu Bajpai1, Siddhartha Datta Gupta, Prasenjit Das
Department of Pathology, Pediatric Surgery1 & Radiology2,
All India Institute of Medical Sciences,
New Delhi, India
Email: prasenaiims@gmail.com
Corresponding Author:
Dr Prasenjit Das
dr_prasenpgi@yahoo.co.in
48uep6bbphidvals|1351 48uep6bbphidcol2|ID 48uep6bbph|2000F98CTab_Articles|Fulltext Hepatocellular adenoma is an uncommon tumor of childhood. It often causes great diagnostic difficulty especially in a child with no known metabolic or inherited liver diseases and in multifocal liver lesions. Radiological features can often be misleading and trucut biopsy may not reveal definite diagnosis. We report a case of multifocal giant hepatocellular adenoma where diagnosis was elusive till the lesion was excised and a wide panel of immunohistochemical tests performed. This index case highlights the need to refer such cases to centers where they can be judiciously worked up.
Case report
The8-year-old girl presented to us with a history of right abdominal lump gradually increasing in size over 2 years with occasional episodes of pain. There was no history of steroid/oral contraceptive intake. Physical examination showed soft non-tender hepatomegaly with sharp margin 10 cm below the costal margin and a 10 cm x10 cm distinctly palpable lobulated right hepatic mass. Hematologic and biochemical parameters were as follows:hemoglobin: 11.5 g/dL, total leucocyte count: 12900/mm3 ,platelet count: 490,000 mm3, blood urea: 25 mg%, serum creatinine: 0.4 mg%, sodium: 137 mEq/L, potassium: 5.2 mEq/L and alpha fetoprotein: 0.60 ng/mL.Liver function tests showed serum bilirubin: 0.6 mg%, protein: 7.5 g%, A/G: 4.8/1.6, SGOT: 65 IU, SGPT: 46 IU and ALP: 114 IU.
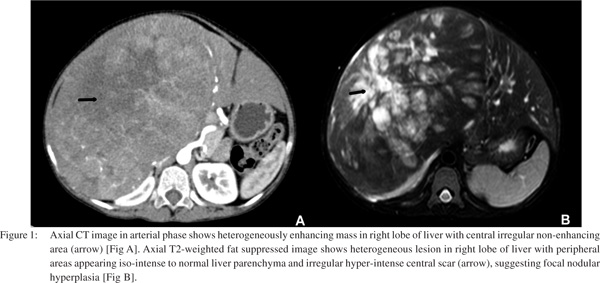
Contrast enhanced computed tomography (CECT) showed a mass involving segments 5,6,7 and 8, abutting and compressing segment 4, but not involving it [Figure1A]. The right branch of the portal and hepatic veins were involved, whilst the main portal vein was not. Splaying of branches of right hepatic artery and middle hepatic vein was also noted. Inferior vena cava and right kidney were compressed by the lesion. Chest imaging was normal. Magnetic resonance imaging (MRI) revealed a large lobulated mass in the right lobe of liver with central T2 hyperintense scar and delayed contrast enhancement, suggestive of focal nodular hyperplasia (FNH) [Figure1B]. A fine needle aspiration was attempted but yielded only blood. This was followed by a trucut biopsy which showed a tiny fragment of hepatic parenchyma with many blood filled spaces which suggested peliosis hepatis. Another biopsy was performed which showed normal looking hepatocytes with maintained architecture and no inflammation. Subsequently, the patient underwent right hepatectomy with a provisional clinico-pathologic diagnosis of FNH. Intra-operatively a 15 cm x15 cm mass was seen in the right lobe of liver with sparing of left lobe of liver.
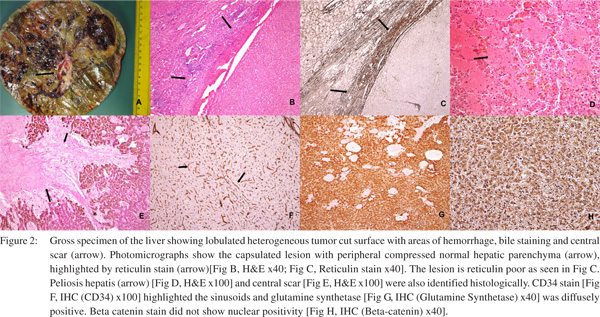
Gross examination showed a single relatively circumscribed unencapsulated lobulated mass measuring 17 cm x17 cm x5cm with greyish green and brown hemorrhagic cystic areas along with an ill-defined central grey white scar and surrounding thin rim of normal parenchyma [Figure 2A]. On microscopy, incomplete fibrous capsule was seen separating the lesion and thin rim of compressed normal parenchyma. Many fibrous septae radiating from the periphery into the lesion were present, but did not show portal tracts or bile ducts. Instead, bile ductular reaction was noted at the interface of lesion and normal due to compression of normal parenchyma [Figures 2B & C].
The lesion itself was reticulin fiber poor. Isolated thick walled arteries were seen in fibrous septae at places. Hepatocytes within the lesion showed extensive intra-cytoplasmic cholestasis and focal macrovesicular steatosis. However, there was no cellular or nuclear pleomorphism and mitoses. In addition, large areas of peliosis hepatis were present in the lesion [Figure 2D]. Sections from the vague gross scar like area showed bland fibrosis surrounded by hepatocytes laden with hemosiderin due to old hemorrhage [Figure 2E]. But there were no portal tracts or bile ducts within it. There after immunohistochemical stains were performed. CD 34 stain highlighted the sinusoidal vascularization [Figure 2F] and Glutamine synthetasestain showed diffuse positivity [Figure 2G]. No nuclear positivity was seen with beta cateninstain [Figure 2H] and serum amyloid A stain was negative. A final diagnosis of hepatocellular adenoma, unclassified type with peliosis hepatis was made. The patient is on regular follow up for 6 months and asymptomatic.
Discussion
Hepatocellular adenoma (HCA) is a rare benign lesion most often seen in young women with history of oral contraceptive use, or in patients taking anabolic steroids and in those with certain inherited metabolic disorders, especially type 1 glycogen storage disease, tyrosinemia, and galactosemia.[1,2] It has been infrequently reported in the pediatric age group and is only incidentally detected throughimaging.[3] However radiological features can often be misleading, especially in children without metabolic disease or in patients without history of medications.[4]HCA can rarely present in children as an asymptomatic mass without any suggestive history. Large adenomas can show central ischemic scars, which may be mistaken radiologically as focal nodular hyperplasia. Trucut biopsy and FNAC in this scenario may not help. Detailed histological examination with use of ancillary techniques is the key to a definitive diagnosis. Large HCA are amenable to rupture, hemorrhage or malignant transformation hence they should be surgically resected in time.
References
- Reddy KR, Schiff ER. Approach to a liver mass. Semin Liver Dis. 1993;13:423–35.
- Resnick MB, Kozakewich HP, Perez-Atayde AR. Hepatic adenoma in the pediatric age group. Clinicopathological observations and assessment of cell proliferative activity. Am J Surg Pathol. 1995;19:1181–90.
- Ramacciato G, Nigri GR, Aurello P, D’Angelo F, Pezzoli F, Rossi S, et al. Giant hepatic adenoma with bone marrow metaplasia not associated with oral contraceptive intake. World J Surg Oncol. 2006;4:58.
- Ribeiro Junior MA, Chaib E, Saad WA, D’Albuquerque LA, Cecconello I. Surgical management of spontaneous ruptured hepatocellular adenoma. Clinics. 2009;64:775–9.
|