48uep6bbphidcol2|ID
48uep6bbphidvals|1719
48uep6bbph|2000F98CTab_Articles|Fulltext
Pseudocyst is a complication of either acute or chronic pancreatitis, which can occur at any site in the abdomen and even in the mediastinum, but the intrahepatic location of pancreatic pseudocyst is a very uncommon event.
1 Till 2016, there have been only 28 reported cases in the literature however none have thus far reported endoscopic ultrasound (EUS) guided management of intrahepatic pseudocysts. Here we report a case series of two patients who presented to us with intrahepatic pseudocysts and of whom the first patient was managed by EUS guided drainage of the pseudocyst.
Case 1
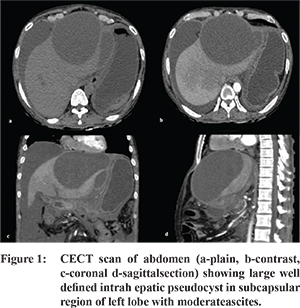
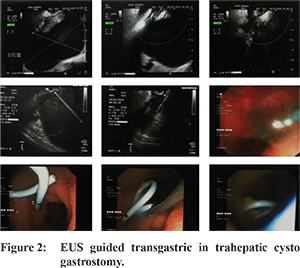
A 45 year old male presented with intermittent epigastric abdominal pain since 1 year which was boring in character, radiating to back. On physical examination he had ascites and left lobe of liver was palpable 3 cm below xiphisternum. Routine blood investigations showed hemoglobin 9.8 gm%, platelet count 215,000/mm3, total leucocyte count4300/mm3, total bilirubin 0.6 mg%, ALT 12 IU/L, AST22 IU/L with serum alkaline phosphatase(ALP) 455 (upper limit of normal 306 IU), serum creatinine 0.9 mg/dl (0.71.2mg/dl). His serum amylase level was 379 IU and serum lipase level was 789 IU. CT scan of the abdomen with pancreas protocol (Figure 1) showed atrophic pancreas with necrosis in head and neck with intrapancreatic and extrapancreatic fluid collection suggestive of walled off collections. Pancreatic duct was measuring 7 mm. There was a large well defined collection seen in subcapsular region of left lobe measuring 14.5x9.2x13 cm which was not communicating with pancreatic duct. Moderate ascites was present. There was complete thrombosis of main, right and left branch of portal vein with cavernoma formation. There was no evidence of any gallstones on ultrasound. Ultrasound guided fine needle aspiration of hepatic cyst fluid showed clear fluid with an amylase level of 12,300 IU/L and a total bilirubin level of 0.6 mg/dL. We performed an EUS,during which EUS guided transgastric cystogastrostomy was done (Figure 2). We placed a 10 french double pigtail stent and another 10 french nasocystic drainage tube. Patient gradually improved and the abdominal pain subsided within a few days. Serial ultrasonograms revealed a progressive decrease in the size of intrahepatic pseudocyst. After 6 weeks of nasocystic drainage placement, complete resolution of pseudocyst was confirmed.
Case 2
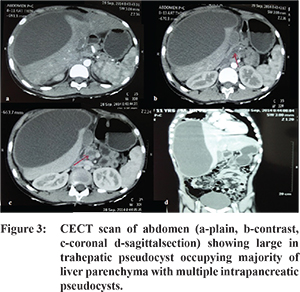
A 10 year old male child presented to us with complaint of right hypochondriac and epigastric abdominal pain since 4 months. He also had previous history of blunt trauma to abdomen 2 years preceeding the presentation. On physical examination, liver was palpable 2 cm below costal margin. His blood investigations including complete hemogram, renal function and liver function test were all within normal limits. His serum amylase level was 179 IU. Ultrasound of abdomen showed large cystic lesion in liver. CT scan of abdomen with pancreas protocol (Figure 3) showed multiple hypodenselesions suggestive of intrapancreatic pseudocysts. There was large intrahepatic cyst occupying majority of liver parenchyma. Percutaneous ultrasound guided aspiration of hepatic cyst fluid showed clear fluid with an amylase level of 5400 IU/L and a total bilirubin level of 0.4 mg/dL. On magnetic resonance cholangio pancreatography (MRCP) there was no pancreatic ductal leakage and the intrahepatic pseudocyst was not communicating with pancreatic duct. Initially we performed USG guided percutaneous drainage with placement of 8 French pigtail catheter. Subsequently, abdominal pain was relieved completely. Follow up ultrasound of abdomen showed gradual shrinkage in size of pseudocyst and complete resolution after 2 weeks.
Discussion
Pancreatic pseudocysts have been well recognized and common complication of both acute and chronic pancreatitis. However, intrahepatic location of pseudocyst have rarely been identified.
1 Less than 30 cases have been reported in the literature till now and all were managed with either percutaneous, endoscopic transpapillary or surgical drainage procedures. Commonly, intrahepatic pseudocysts are single and involve left lobe of liver. However, multiple and right lobe intrahepatic pseudocysts have also been described.
1,2 The pathophysiology of intrahepatic pseudocysts can be explained by two mechanisms.
2 The first proposed mechanism, likely in our first case, is leakage of the pancreatic juice in prerenal space and there after eroding through the posterior layer of the parietal peritoneum and into the lesser sac. Lesser sac collection then follow the path along the lesser omentum or gastrohepatic ligament toward the liver leading to the formation of left lobe subcapsular collections. Second mechanism, likely in our second case, is tracking of pancreatic juice along the hepatoduodenal ligament from the head of pancreas to the portahepatis resulting in formation of intrahepatic parenchymal collections. Pseudocysts, which form as per the first mechanism, are mainly subcapsular in location and are biconvex in shape. Intra parenchymal pseudocysts formed as a result of the second mechanism are located away from the liver capsule and are located near branches of porta hepatis. Intrahepatic pseudocysts pose a diagnostic challenge because they are rarely considered in the differential diagnosis of cystic hepatic lesions. Amylase rich fluid on aspiration and communication of pseudocyst with disrupted pancreatic duct on imaging is indicative of diagnosis. However, neither of pseudocysts in our two cases had communication with pancreatic duct.
There is no consensus regarding the management of intrahepatic pseudocysts. Majority of the intrahepatic pseudocysts have been managed by either surgical, radiologically guided percutaneous drainage/aspiration or ERCP guided transpapillary drainage.
3-5 EUS guided management of intrahepatic pseudocyst has never been reported in literature. We managed our first case of intrahepatic pseudocyst successfully by EUS guided transgastric cystogastrostomy alone. We managed our second case of intrahepatic pseudocyst with percutaneous drainage, as pediatric EUS endoscope was not available.
References
- Mofredj A, Cadranel JF, Dautreaux Met al. Pancreatic pseudocyst located in the liver: a case report and literature review. J Clin Gastroenterol. 2000;30:813.
- Okuda K, Sugita S, Tsukada E, Sakuma Yet al. Pancreatic pseudocyst in the left hepatic lobe: a report of two cases. Hepatology. 1991;13:359-63.
- Kralik J, Pesula E. A pancreatic pseudocyst in the liver. Rozhl Chir. 1993;72:913.
- Bhasin DK, Rana SS, Chandail VS et al. An intrahepatic pancreatic pseudocyst successfully treated endoscopic transpapillary drainage alone. JOP. 2005;6:5937.
- Atia A, Kalra S, Rogers M et al. A wayward cyst. JOP. J Pancreas (Online) 2009;10:4214.