48uep6bbphidcol2|ID
48uep6bbphidvals|1745
48uep6bbph|2000F98CTab_Articles|Fulltext
Tuberculosis (TB) is a major public health problem in India with an estimated 50000 deaths per year.
1 Gastrointestinal TB though not as common as pulmonary TB, continues to be a major cause of morbidity. Isolated colonic TB is rare with only 10.8% of patients with gastrointestinal TB having isolated colonic involvement.
2 Isolated rectal TB is still rarer accounting for 5% of cases of gastrointestinal TB. The majority of patients present with nonspecific symptoms including the weight loss and abdominal pain.
3 Endoscopic and radiological features are also nonspecific and frequently mimic malignancy or inflammatory bowel disease.
4 Owing to its rarity as well as nonspecific endoscopic and radiological characteristics, isolated colorectal tuberculosis is frequently misdiagnosed as malignancy. In addition, it has been observed that tuberculosis and carcinoma can coexist.
5 Prompt diagnosis and correct treatment is essential since both the diseases have significant treatment related toxicities and delays in instituting the correct treatment can worsen the morbidity. We present a series of patients referred to our center with suspected diagnosis of colorectal carcinoma and who were diagnosed to have isolated colorectal tuberculosis.
Case Series
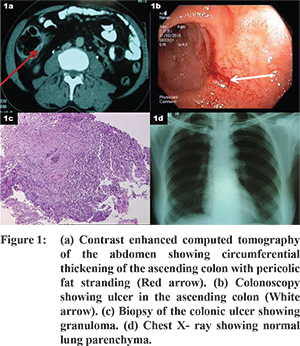
This is a retrospective review of a series of 6 cases of isolated colorectal tuberculosis presenting to the colorectal clinic at Tata Memorial Hospital. Median age at presentation was 32 years (range: 33-51 years). There were 4 males and 2 females in our series. None of the patients had prior history of pulmonary or extra pulmonary tuberculosis. Four patients had ill-defined abdominal pain and significant weight loss whereas two patients had history of recurrent sub-acute intestinal obstruction. None of the patients except one with rectal ulcer had history of rectal bleeding. Only two patients had a palpable mass per abdomen. Contrast enhanced computed tomography (CECT) of the abdomen was done in all the patients and showed circumferential bowel thickening with or without stricture, pericolic fat stranding and pericolic nodal masses (Figure 1a). On colonoscopy, sub-site of tuberculosis was predominantly in the right colon (ascending colon in two patients, hepatic flexure in three patients and rectum in one patient). Colonoscopic findings included stricture in four patients and solitary ulcer in the other two patients (Figure 1b). Due to this, ileum could be intubated only in two patients; findings were inflamed mucosa in one patient and normal mucosa in the other patient. There was no evidence of ulcer or stricture in the terminal ileum in either of the patients. Diagnosis was established based solely on the detection of granuloma on biopsy specimen at histopathological examination (Figure 1c) in all the patients. Neither AFB staining nor mycobacterial culture was done to establish the diagnosis. None of the patients had coexistent colorectal cancer.Routine blood investigations revealed leukocytosis in two patients whereas they were normal in the rest. None of the patients had anemia. CarcinoEmbryonic Antigen (CEA) report was available in 4 patients with CEA levelswithin normal limits for 3 patients (Mean - 4.28; Range 0.64 - 8.75IU/L). Chest X ray did not reveal any abnormality in any of the patients (Figure 1d). All 6 patients were treated with anti-tubercular therapy for 6-12 months, though two patients required segmental colonic resection before the start of therapy as they had presented with recurrent sub-acute intestinal obstruction. Both patients who underwent surgery didnot have a definitive diagnosis prior to surgery. Intra operatively there was no evidence of tubercles, gross mesenteric lymphadenopathy or ascites. None of the patients in the series had significant anti tuberculous treatment related toxicity and compliance with the treatment was 100%. Median follow up of these patients was 18 months (range: 12-60 months). All patients had complete clinical resolution of symptoms.
Discussion
According to a recent World Health Organization (WHO) report, global annual incidence of tuberculosis is estimated to be around 9.4 million cases, of which 1.98 million cases are from India.
6 There is resurgence of the cases of tuberculosis in the developed countries secondary to increase in the prevalence of immunocompromised individuals. Isolated colonic tuberculosis is rare accounting for 10.8% of all the cases of gastrointestinal tuberculosis. The most commonly affected site is the transverse colon, followed by the rectum and the ascending colon.
2 None of the patients in the present series had prior history of pulmonary or extra pulmonary tuberculosis which is consistent with the literature where in less than 25% of patients with gastrointestinal tuberculosis have concomitant pulmonary tuberculosis.
Owing to the rarity of isolated tuberculosis of the colon and nonspecific clinical, radiological and endoscopic characteristics, these cases can be misdiagnosed as colorectal carcinoma or inflammatory bowel disease. Endoscopic biopsy may not be diagnostic particularly in cases of stricture where ulcerated areas may not be accessible. In addition, tuberculosis and cancer may coexist further complicating the diagnosis as well as treatment.
5 As Tata Memorial Hospital is a referral oncology center, we see many patients with uncertain diagnosis who are referred to rule out malignancy. In the present series diagnosis could not be established despite colonoscopic as well CECT abdomen directed percutaneous biopsies in two of the patients. In view of clinical suspicion as well as history of recurrent sub-acute intestinal obstruction, segmental colonic resection was performed in them. Diagnosis was established on the final histopathological examination of the resected specimen in both these patients. In the case of another patient, repeat colonoscopy with biopsy was required to establish the diagnosis of tuberculosis. This stresses the importance of generous well directed biopsy as well as use of AFB stain and mycobacterial culture whenever possible if the biopsy fails to confirm a diagnosis of malignancy in all suspected cases. Thus, isolated colorectal TB, though rare, is an important differential diagnosis to malignancy in India where TB is endemic. A high index of suspicion and well directed biopsies for histopathological and mycobacterial evaluation are the key to prevent delay in the diagnosis.
References
- Khatri GR, Frieden TR. Controlling tuberculosis in India. N Engl J Med. 2002 Oct 31;347(18):1420-5.
- Nagi B, Kochhar R, Bhasin DK, Singh K. Colorectal tuberculosis. Eur Radiol. 2003;13(8):1907-12.
- Mukewar S, Mukewar S, Ravi R, Prasad A, S Dua K. Colon tuberculosis: endoscopic features and prospective endoscopic follow-up after anti-tuberculosis treatment. Clin Transl Gastroenterol. 2012;3:e24.
- Alvares JF, Devarbhavi H, Makhija P, Rao S, Kottoor R. Clinical, colonoscopic, and histological profile of colonic tuberculosis in a tertiary hospital. Endoscopy. 2005;37(4):351-6.
- Kaushik R, Sharma R, Attri AK. Coexisting tuberculosis and carcinoma of the colon: a report of two cases and a review of the literature. Trop Gastroenterol. 2003;24(3):137-9.
- WHO. Global Tuberculosis Control - Epidemiology, Strategy, Financing. WHO, 2009, pp 411 (WHO/HTM/TB/2009).