48uep6bbphidcol2|ID
48uep6bbphidvals|1759
48uep6bbph|2000F98CTab_Articles|Fulltext
Hydatid cysts are a common health problem in endemic areas. The presentation of a hydatid cyst varies based on its location.
1 Untreated or inadequately treated hydatid cyst maylead tocomplications, like infection, rupture and obstructive jaundice.
2,3 A hepatic artery pseudoaneurysm secondary to infection of a hydatid cyst is a rare complication.
3 We report such a case and its successful endovascular management.
Case Report
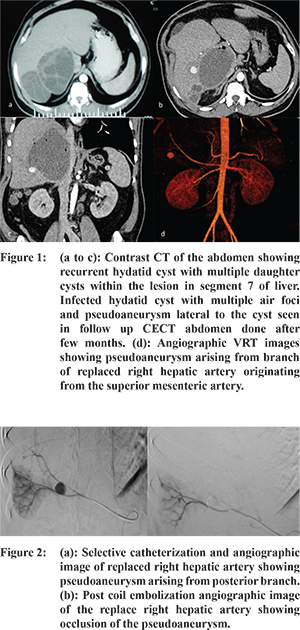
A 38 year old male with history of hepatic hydatid cyst presented with mild fever and pain abdomen. He was referred for radiologic evaluation. He had beenon oral albendazole therapy for the past two months. No history of intervention could be elucidated. A computed tomography (CT) scan performed at the time of initial diagnosis (Figure 1) showed a well-defined cystic lesion with multiple septae, suggestive of a hydatid cyst. There was no evidence of biliary dilatation or gas in the cyst. Ultrasonography performed in our department revealed a multiseptate cyst alongwith daughter cystsin the right lobe of the liver, consistent with hydatid cyst disease. In addition, a small berry like anechoic cystic lesion was seen close to the wall of the hydatid cyst. The lesion showed colour filling, turbulent flow, yin-yang sign and bidirectional flow pattern on colour duplex imaging, confirming a pseudoaneurysm. However, there was no evidence of rupture of the cyst. Subsequent CT angiography revealed a large hydatid cyst in the right lobe of the liver with thick enhancing irregular wall.Air foci were found within as well as adjacent to the wall suggesting the possibility of a secondary infection of the cyst. The pseudoaneurysm was seen as a small well defined contrast filled area adjacent to the cyst wall with attenuation of hepatic artery. The volume rendered CT angiography image taken in the arterial phase (Figure 1) showed that the pseudoaneurysm was arising from the posterior division of the replaced right hepatic artery which originated from the superior mesenteric artery (SMA). Based on these imaging features, a diagnosis of secondarily infected hydatid cyst leading to hepatic artery pseudoaneurysm was made. Patient’s gastric aspirate did not reveal any evidence of hemobilia and there was no drop in his hemoglobin level. Hence, he was electively taken for pseudoaneurysm embolization the next day through femoral route. Based on the VRT image, the SMA was selectively catheterised to enter the replaced right hepatic artery (Figure 2). The posterior branch was super selectively catheterised using a microcatheter (Progreat) and the pseudoaneurysm was embolized successfully using Hilalmicro coils (Figure 2). No procedure related complications were noted. Follow up ultrasonography with duplex study done after a week was unremarkable. Surgical management of the hydatid cyst was done subsequently. Serial follow up ultrasonography one month apart was unremarkable and patient is asymptomatic on follow up for the last one month.
Discussion
The most common complication of a hydatid cyst is infection and symptoms may vary with different (latent, subacute or acute) presentations.
2 Other common complications are obstructive jaundice by mass effect; pleural, peritoneal or intrabiliary rupture of cyst; cholangitis; pancreatitis and portal vein thrombosis. Intrahepatic vascular complications are very rare with only a few cases reported in the medical literature.
2,4 In this case, secondary infection and inflammation of the hydatid cyst might have involved the adjacent right hepatic artery resulting in weakness of arterial wall, leading to pseudoaneurysm. Due to the risk of life threatening bleed, the patient was taken up for embolization. This pseudoaneurysm which had a narrow neck was successfully treated with microcoils.
References
- Sachar S, Goyal S, Goyal S, Sangwan S. Uncommon locations and presentations of hydatid cyst. Ann Med Health Sci Res. 2014;4(3):447-52.
- Derbel F, Ben M, Hadj Hamida MB, Mazhoud J, Youssef S, Ben A, et al. Hydatid Cysts of the Liver - Diagnosis, Complications and Treatment. Abdominal Surgery.; 2012. Available from: http://www.intechopen.com/books/abdominal-surgery/hydatid-cysts-of-the-liver-diagnosis-complications-and-treatment. [cited 2014 Sep 30].
- Lakshminarayan R, Anuradha C. Haemobilia - a rare presentation of intrabiliary hydatid disease: Intrabiliary hydatid presenting as haemobilia. J Med Imaging Radiat Oncol. 2012;56(6):650-3.
- Alexiou. Complications of Hydatid Cysts of the Liver: Spiral Computed Tomography Findings. Gastroenterol Res. 2012; Available from: http://www.gastrores.org/index.php/Gastrores/article/view/478. [cited 2014 Sep 30].