48uep6bbphidcol2|ID
48uep6bbphidvals|1762
48uep6bbph|2000F98CTab_Articles|Fulltext
Primary hepatic angiosarcoma is rare, and accounts for 0.1%-2% of all malignant primary liver tumours, and is commoner in elderly males.
1 Presentation may range from asymptomatic detection to widely disseminated disease at diagnosis.
2 In absence of history of exposure to carcinogens including thorotrast, arsenicals, vinyl chloride monomer and radiation, especially in a young adult, this entity may not be considered in differential diagnoses.
2 By the time this tumour produces any symptoms, it is already extensive with overall survival often less than a year.
3 Its bad prognosis may also be attributed to its high recurrence rate and resistance to traditional chemotherapy and radiotherapy.
4,5 We herein describe a case of hepatic angiosarcoma detected in a young male patient, with an apparently innocuous presentation that belied the extent of hepatic involvement.
Case Report
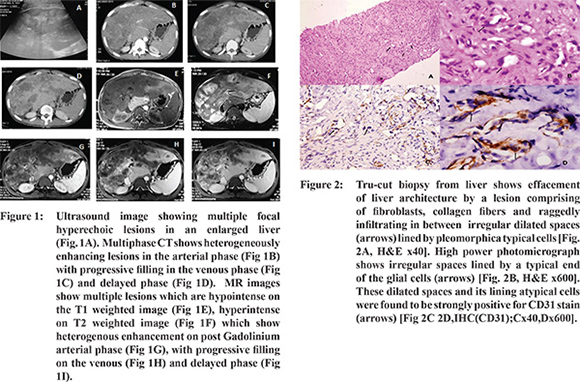
A 25 years old gentleman, native of Bihar, India, presented to the outpatient department with sensation of heaviness in the upper abdomen over the past 6 months. He had noticed jaundice for the past one month.There was no exposure to vinyl chloride, thorium (thorotrast), arsenic or radiation. A large hard and irregular hepatomegaly extending upto the umbilicus was palpable. His blood investigations revealed: hemoglobin of 10 g/dl, total leukocyte count 8200/mm3 and platelet count 143x103/mm3. Liver function test revealed total/conjugated bilirubin of 4.1/3.6 mg/dl, total protein 8.0 g/dl, albumin 3.8 g/dl, elevated aspartate aminotransferase 203 IU/L (normal < 40 IU/L), alanine aminotransferases 122 (normal < 40 IU/L) and alkaline phosphatase 1480 IU/L (normal < 280 IU/L). His viral markers (HBsAg, total anti-HBcAb, anti HCV Ab and HCV RNA) were negative. Additional tests, including prothrombin time and tumour markers like alfa-fetoprotein, carcinoembryonic antigen and CA 19-9 were within normal limits. Endoscopy revealed high grade esophageal varices. Ultrasound showed hepatomegaly with multifocal hyperechoic lesions. On multiphase computed tomography (CT) and subsequent magnetic resonance imaging (MRI), these lesions showed heterogeneous enhancement in the arterial phase, progressively filling in on venous and delayed phases (Figure 1). Liver biopsy revealed infiltration of hepatic parenchyma by irregular slit like vascular spaces lined with pleomorphic atypical cells revealing high nucleo-cytoplasmic ratio, hyperchromatic nuclei and moderate nuclear pleomorphism. Areas of collagenisation were noted in between these infiltrating foci (Figure 2A, 2B). Immunohistochemistry stains for CD 31 and CD 34 were positive whereas the tumour was negative for cytokeratin (Figure 2C, 2D). Hepatic iron deposition was not noted. Overall histomorphological features and immunohistochemical results were compatible with a diagnosis of hepatic angiosarcoma. Due to large tumour bulk involving both lobes of liver, abnormal liver function and associated portal hypertension, the patient was advised supportive care only.
Discussion
Despite being the most common primary malignant mesenchymal tumour of the liver, hepatic angiosarcoma is uncommon and constitutes approximately 2% of all primary liver tumours. A strong male predominance (male: female ratio of 4:1) has been reported.
1 Though common age at presentation is 60-70 years, younger individuals may also be affected. Association with exposure to various carcinogens (thorotrast, vinyl chloride, arsenic compounds) as well as to anabolic steroids, along with an association with hemochromatosis and neurofibromatosis-1 have been described.
2 However, cases may occur in the absence of exposure. Upto 40% cases clinically and radiologically mimic advanced hepatic fibrosis or cirrhosis, as can be seen at autopsy series4; however, the association between chronic liver disease and angiosarcoma is not clearly established. Four patterns of hepatic angiosarcoma have been described multiple nodules, a large dominant mass, a large focal liver lesion and a diffuse infiltrating micronodular form. Dynamic multiphase CT or MR imaging reflects the hypervascular nature of these tumours, typically with peripheral enhancement in the hepatic arterial and portal venous images, and progressive enhancement on the delayed (equilibrium phase) images. Imaging features may overlap with those of cavernous hemangiomas, hypervascular metastases or hepatocellular carcinomas. Some features that suggest the possibility of hepatic angiosarcoma include presence of tumour heterogeneity and hemorrhage, bizarre areas of enhancement, persistent but heterogeneous enhancement which is less than that of the aorta or hepatic artery.
5 Absence of ‘washout’ on the equilibrium phase images helps to differentiate this tumour from hepatocellular carcinoma. However, in small lesions radiological features may not be classical. While imaging such as CT and MRI can be helpful, but is often not conclusive. FDG-PET has also been used. Therapeutic options available are liver resection and chemotherapy. Liver transplantation has not so far been reported to be significantly beneficial for this subgroup of sarcoma patients. However, high recurrence rate and resistance to chemo-radiotherapy increase morbidity. Lungs are the most common site of metastasis followed by spleen and bones.
4
References
- Mani H, Van Thiel DH. Mesenchymal tumors of the liver. Clinics in liver disease. 2001;5(1):219-57. Epub 2001.
- Molina E, Hernandez A. Clinical manifestations of primary hepatic angiosarcoma. Digestive diseases and sciences. 2003;48(4):677-82. Epub 2003.
- Stambo GW, Guiney MJ. Hepatic angiosarcoma presenting as an acute intraabdominal hemorrhage treated with transarterial chemoembolization. Sarcoma. 2007;90:169.Epub 2008.
- Locker GY, Doroshow JH, Zwelling LA, Chabner BA. The clinical features of hepatic angiosarcoma: a report of four cases and a review of the English literature. Medicine. 1979;58(1):48-64. Epub 1979.
- Koyama T, Fletcher JG, Johnson CD, Kuo MS, Notohara K, Burgart LJ. Primary hepatic angiosarcoma: findings at CT and MR imaging. Radiology. 2002;222(3):667-73. Epub 2002.