48uep6bbphidcol2|ID
48uep6bbphidvals|1765
48uep6bbph|2000F98CTab_Articles|Fulltext
Adult intussusception is a rare entity and can involve any site from stomach to rectum. It accounts for 1 to 5% of cases of intestinal obstruction and mean age of presentation is around 50 yrs. The most common site is the small bowel followed by the large bowel and rarely the stomach. An identifiable aetiology is present in 80 to 90% of adult intussusceptions and considerable variation is seen for each of these sites.
1 Causes may be benign or malignant.
Case Report
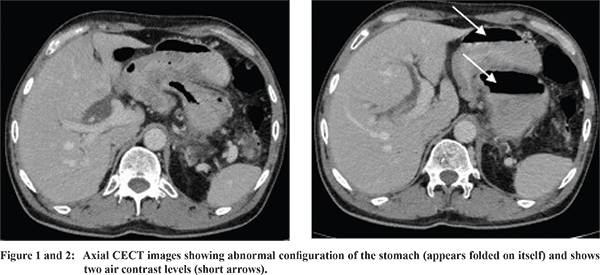
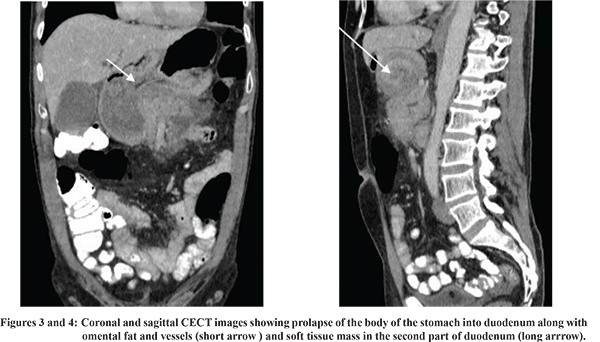
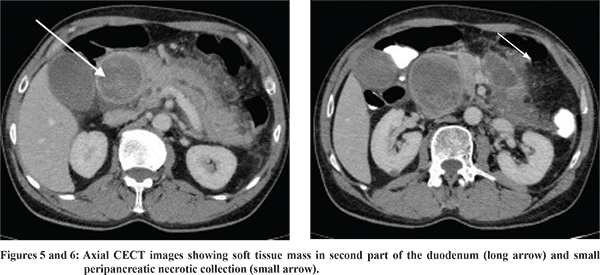
A 65-year old male presented with pain abdomen in the epigastrium for 6 months associated with intermittent vomiting and acute exacerbation of pain radiating to the back for the last 10 days. USG abdomen revealed a bulky and heterogeneous pancreas. So, the possibility of acute pancreatitis was considered and CECT abdomen was performed for further evaluation which revealed an abnormal configuration of the stomach with two air contrast levels (Figure 1 and 2) and a well-defined soft tissue density mass lesion in the antrum of the stomach prolapsing into the dilated D1 and D2 part of the duodenum with narrowing and foreshortening of the body of the stomach telescoping into the duodenum along with omental fat and vessels (Figure 3 and 4). D3 and D4 parts of the duodenum appeared normal. The pancreas was enlarged with diffusely hypo-attenuating pancreatic parenchyma and extensive peri-pancreatic fat stranding. A small ill-defined necrotic peri-pancreatic collection was also seen (Figure 5 and 6). Common bile duct and the main pancreatic duct were dilated likely due to mass effect by the prolapsing gastric mass on the second part of the duodenum containing the ampulla of Vater. The gall bladder and CBD contain hyper-dense contents likely sludge. Serum amylase level at admission was 747 U/L (normal 28-100U/L) which was in concordance with acute pancreatitis. The patient was subjected to an upper GI endoscopy which revealed a large fleshy submucosal mass in the antrum extending into the second part of the duodenum and the scope could not be negotiated beyond this. Biopsies taken during the UGI endoscopy did not reveal any malignant cells. The patient underwent an exploratory laporotomy and intraoperatively, the surgeon noted a gastro-gastric intussusception with firm submucosal growth along the lesser curvature at the incisura prolapsing into the D2 segment of the duodenum. The intussusception was reduced and a distal gastrectomy followed by a Billroth I reconstruction and cholecystectomy was done. Post-operative histopathology revealed a gastrointestinal stromal tumor (GIST) of the stomach. The patient recovered well and no morbidity was encountered during the post-operative period.
Discussion
The most common benign causes of small bowel intussusception include lipoma, leiomyoma, adenomatous polyp, Meckel’s diverticulum, GIST and lymphoid hyperplasia while the malignant causes include lymphoma, malignant GIST and metastasis. Causes of large bowel intussusception are similar to those of small bowel in addition to primary adenocarcinoma, leiomyosarcoma, Crohn’s disease and mucocele of the appendix.Benign causes acting as lead points in gastric intussusception are adenoma, polyps, leiomyoma, lipoma, hamartoma and malignant causes are adenocarcinoma and leiomyosarcoma.
2 Common presenting symptoms of intussusception are abdominal pain, nausea, and vomiting; less frequently, fever, melena, weight loss and constipation.
2 In our case, the patient is a non-alcoholic and the presentation was that of acute on chronic pain abdomen with the cause of acute pain being acute pancreatitis. The acute pancreatitis was most likely caused due to mass effect of the telescoping gastric mass into the first and second part of the duodenum obstructing the drainage of the common bile duct and the main pancreatic duct at the duodenal papilla in the second part of the duodenum. Bowel obstruction is rare and usually presents with pancreatitis due to obstruction of the ampulla of Vater which is very rare. Literature searches showed several case reports of a gastric polyp causing acute pancreatitis
3 and very few case reports of a gastric GIST presenting with pancreatitis.
4,5
References
- Agha FP. Intussusception in adults. AJR. 1986;146:527-31.
- Gayer G, Zissin R, Apter S, Papa M, Hertz M. Pictorial review : adult intussusception - a CT diagnosis. Br J Radiol. 2002;75:185-190.
- Galeano-Cassaz C, Bonnet S, Chereau N, Dousset B, Lamarque D, Douard R. Gastric polyp prolapsed into the duodenum as a rare cause of acute pancreatitis. Ann R CollSurg Engl. 2010;15.
- Senadhi V., Arora D., Jani N. Gastrointestinal stromal tumor (GIST) presenting with acute pancreatitis. Endoscopy. 2011;43:E76.
- Jones O, Monk D, Balling T, Wright A. Acute pancreatitis secondary to a prolapsed gastric fundal GIST. Int J Surg Case Rep. 2012;3(2):82-5.