mixing zoloft and weed mixing ibuprofen and weed click here
Department of Surgery1 and MorbidAnatomy2
Obafemi Awolowo University
Teaching Hospitals Complex
PMB 5538, Ile-Ife, Nigeria.
Corresponding Author:
Dr. Adewale O Adisa
E-mail: wadisc@yahoo.com
Abstract
Background: Gastrointestinal schistosomiasis may involve the appendix and there is nospecific clinical picture associated with the same.
Methods: The clinical records and histopathological slides of all patients diagnosed withschistosomal appendicitis between January 1989 and December 2006 in Ile-Ife, south westNigeria, were reviewed.
Result: Of 956 patients who had appendectomy at the Obafemi Awolowo University TeachingHospital within the study period, 22 (2.3%) had histopathological diagnosis of schistosomalappendicitis. Eighteen (81.8%) were male whilst 4 (18.2%) were female. Their ages rangedbetween 15 and 63 years with a mean of 28.2 (+5.6) years. The mean duration of right lowerquadrant abdominal pain was 4.2 years. Appendiceal and periappendiceal adhesions werenoted intraoperatively in 17 (77.3%) and the appendix was adjudged grossly inflamed in 9(40.9%) patients. Submucosal fibrosis and eosinophilia were the common histopathologicalfindings aside from submucosal oviposition. All patients received antischistosomal drugsand one patient developed adhesive intestinal obstruction 9 months after surgery.
Conclusion: Schistosomal appendicitis may present acutely but diagnosis is only reliablymade at histopathological examination. Adequate follow-up is however required to ascertainlong-term outcome
|
48uep6bbphidvals|179 48uep6bbphidcol4|ID 48uep6bbph|2000F98CTab_Articles|Fulltext Schistosomal infections are on the increase in some endemicareas across Africa.[1,2] This chronic granulomatous infection,induced by ova deposition, may involve different parts of thegastrointestinal tract; the ileocaecal region is one of the mostcommon sites involved. The appendix may be involved in upto two-thirds of cases; however the clinical manifestation varieswidely amongst patient.[3,4] The resulting ova deposition in theappendix usually leads to the development of a proliferativegranulomatous response especially within the mucosal andsubmucosal layers of the appendix along with submucosallymphoid hyperplasia.[3,5,6] The granulomas may later bereplaced by varying degrees of submucosal fibrosis.[5,7] At anyof these stages, the patient may present with features of acuteappendicitis.
This study reviews the clinical features as well as theoperative and pathological findings in patients withschistosomal appendicitis in our hospital.
Methods
This study was conducted at Obafemi Awolowo TeachingHospitals Complex Ile-Ife which is located in Osun state andserves the health needs of the urban and largely agrarianpopulation of some parts of southwestern Nigeria. It servesas a referral centre to many hospitals in Ondo, Ekiti,Oyo and Osun states. The clinical records of all patients whohad undergone appendectomy following a clinicaldiagnosis of acute or subacute appendicitis at the Ife Hospitalunit of the Obafemi Awolowo University Teaching HospitalComplex in south western Nigeria between January 1989 andDecember 2006 (15-year period) were reviewed. Preoperativeclinical features, investigation and intra-operative findings aswell as the pathologist’s reports of the histological slidesindicating schistosomal appendicitis were also reviewed.Data extracted were subjected to descriptive analysis usingthe Statistical Package for Social Sciences (SPSS)version 13.
Results
Within the study period, a total of 956 patients underwentappendectomy for acute and subacute appendicitis. Of these22 (2.3%) had schistosomal appendicitis. They were 18 maleand 4 female patients with an age range of 15-16 years (Mean:28.2 years). Half of the patients including all 4 females were25 years or less in age (Table 1).
All patients suffered right lower quadrant abdominal pain.Other associated symptoms include nausea in 8 (36.4%),fever in 7 (31.8%) and vomiting in 3 (13.6%) as shown inTable 2. Varying degrees of tenderness in the right lowerquadrant of the abdomen were recorded in 18 of the patients.However, the duration of different symptoms ranged between2 days to 3 weeks with a mean duration of 14 days.
Preoperative differential white cell count demonstratedeosinophilia in two-thirds of the patients, lymphocytosis inone half of them and neutrophilia in 9.1%. All patients hadabdominal ultrasound which reported right iliac fossa probetenderness in 10 (45.5%), periappendiceal fluid collection in7 (31.8%), appendiceal wall thickening in 5 (22.7%) andhepatomegaly in one patient. Subsequently, emergency openappendectomy was done in 15 patients whilst 7 patients whopresented with longer duration of symptoms had electiveprocedures. Intraoperative findings include appendiceal andperiappendiceal adhesions in 11 (50%), mesoappendiceallymphadenopathy in 3, and the appendix was adjudged to begrossly inflamed in 9 (40.9%) patients. Only one patient hadpostoperative wound infection in the form of a stitch sinus. Onreceiving the histopathological report, all patients underwenttreatment with a single 60 mg/kg dose of oral praziquantel.Duration of follow up ranged between one and 12 monthswith a mean of 2.2 months. One female patient presentedwith features of adhesive intestinal obstruction 9 months aftersurgery and did well on conservative management.
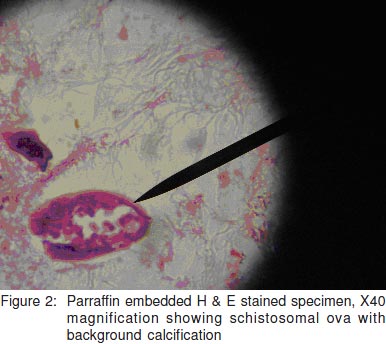
A review of the histopathological slides of the patientsrevealed schistosomal ova in the submucosal layer in allpatients [Figures 1 and 2]. Ova were also seen in themuscularis propria and serosal layers in 7 (31.8%) patients.Submucosal eosinophilia was noted in 20 (90.9%) andsubmucosal fibrosis in 16 (72.7%). Eight patients (36.4%)had suppurative inflammation whilst granulomas were seenin 13 (59.1%) patients.


Discussion
In this study, schistosomal appendicitis occurred in 2.3% ofpatients with acute appendicitis. This is relatively highercompared to 1.5%[5] and 1.3% from different regions of SaudiArabia,[4] but is lower than 3.5% reported from Dar’es Salam inTanzania.[8] The true incidence of schistosomal infestation inthe south western region of Nigeria is not known and thisfinding may point towards a high prevalence rate. Similar tofindings in previous reports,[4,5,9] a male predominance with amean age of 28.2 years was observed in this study. A similarmean age was seen in the African-American patientpopulation.[10] In our own developing economy, young malepatients are more involved in outdoor occupations especiallywith a large proportion of our patients being farmers with ahigher probability of exposure to schistosomiasis than thefemale population or the older age groups.
All patients presented with features suggestive of acuteappendicitis and complaints of right lower quadrant abdominalpain of varying duration. Although a mean duration of symptomsof 14.2 days before presentation is relatively higher than whatwe have observed in our patients with non-schistosomal acuteappendicitis, no other symptom or signs in the patients pointed to schistosomiasis preoperatively. This is in keeping withreports of previous studies.[11,12,13] The investigations carried outon our patients were mainly those for diagnosis of routineacute appendicitis and it is not surprising that diagnosis ofschistosomal appendicitis was not entertained in any of thepatients, preoperatively. Microscopic examination of a freshrectal biopsy is helpful in diagnosing acute gastrointestinalschistosomal infestation and this would have been of value indistinguishing acute from chronic schistosomal conditionswith implications for treatment following surgery, but this wasnot done in our patients.
Findings on review of the histopathologic slides showfeatures suggestive of chronic schistosomal infection of theappendix in many patients. These include submucosal fibrosisin about three-quarters of the studied specimen. This is similarto the report of a previous study in Saudi Arabia onschistosomal appendicitis highlighting submucosal fibosisas a very common finding.[5] The other common features includesubmucosal lymphoid hyperplasia or atrophy and submucosalor serosal granuloma.[14,15] Many studies had questioned therelevance of schistosomiasis in appendicitis with someauthors postulating that it may actually be a mere histologicalcoincidence.[16,17,18] However in the majority of our patients, ahistory of abdominal pain suggests chronicity of the condition.The histopathological slides also show chronic inflammatorycells and fibrosis commonly seen in chronic appendicitis. Itmay therefore be that previously existing schistosomalinfestation induces a chronic inflammatory process in theappendix as in other parts of the gastointestinal tract but theresultant fibrosis and stricture formation with partial luminalobstruction of the appendix may present as acute appendicitisto the surgeon.
The average duration of follow up was 2.2 months. Onefemale patient presented with adhesive intestinal obstructioneight months after surgery. She had stopped attending theout-patients’ clinic for six months before re-presenting. Shewas however managed conservatively and did wellsubsequently. The long-term outcome of other patients couldnot be ascertained.
Conclusion
Schistosomal appendicitis is rare but may present acutely.For a reliable diagnosis histopathological examination is aprerequisite. The outcome of surgery and treatment is good ifpatients are treated promptly.
References
-
Duvie SOA, Diffang C, Guiguis MN. The effect ofschistosoma haematobium infestation on the vermiformappendix: the Nigerian experience. J Trop Med Hyg.1987;90:13–8.
-
Adebamowo CA, Akang EE, Ladipo JK, Ajao OG.Schistosomiasis of the appendix. Br J Surg.1991;78:1219–21.
-
Gelfand M, Ross CM, Blair DM, Castle WM, Weber MC.Schistosomiasis of the male pelvic organs. Severity ofinfection as determined by digestion of tissues andhistologic methods in 300 cadavers. Am J Trop Med Hyg.1970;19:779–84.
-
Abu-Eshy SA, Malik GM, Khan AR, Khan GM, Al-Shehri MY.Schistosomal appendicitis. Ann Saudi Med.1995;15:347–9.
-
Meshikhes AW, Chandrashekar CJ, Al-Daolah Q, Al-Saif O,Al-Joaib AS, Al-Habib SS, et al. Schistosomal appendicitisin the Eastern Province of Saudi Arabia: Aclinicopathological study. Ann Saudi Med. 1999;19:12–4.
-
Bell DR. Blood flukes- schistosomes. In: Lecture notes ontropical medicine. London: Blackwell Scientific,1981:187–209.
-
Hodasi M. Schistosomal appendicitis. Trop Doct.1988;18:105–6.
-
Mbembati NA, Lema LE, Mwakyoma HA, Ussiri EV.Appendicitis in Dar’es Salaam, histological pattern. CentAfr J Med. 1996;42:68–70.
-
Al-Kraida A Giangreco A, Shaikh MU, Al-Shehri MY.Schistosomal appendicitis. Br J Surg 1988;75:58–60.
-
Nandipati K, Parithivel V, Niazi M. Schistosomiasis: a rarecause of acute appendicitis in the African Americanpopulation in the United States. Am Surg. 2008;74:221–3.
-
Lowenthal MN. Schistosomal appendicitis. Isr Med AssocJ. 2005;7:679.
-
Khan GM, Grillo IA, Abu-Eshy SA, Khan AR, Mubarak J,Jastaniah S. Pathology of the appendix. J Natl Med Assoc.2000;92:533–5.
-
Adehossi E, Parola P. Schistosomal appendicitis. LancetInfect Dis. 2004;4:498.
-
Babekir AR, Devi N. Analysis of the pathology of 405appendices. East Afr Med J. 1990;67:599–602.
-
Ojo OS, Udeh SC, Odesanmi WO. Schistosomiasis of theappendix. Review of the histopathological findings inappendices removed for acute appendicitis in Nigerians. J R Coll Surg Edinb. 1991;36:245–8
-
Satti MB, Tamimi DM, Al Sohaibani MO, Al Quorain A.Appendicular schistosomiasis: a cause of clinical acuteappendicitis? J Clin Pathol. 1987;40:424–8.
-
Doudier B, Parola P, Dales JP, Linzberger N, Brouqui P,Delmont J. Schistosomiasis as an unusual cause ofappendicitis. Clin Microbiol Infect. 2004:10:89–91.
-
Kakande I, Nehra MK. Appendicectomy in ConsolataHospital, Nyeri: analysis of operative and histologicalfindings. East Afr Med J. 1990;67:573–7.
|