48uep6bbphidcol2|ID
48uep6bbphidvals|1939
48uep6bbph|2000F98CTab_Articles|Fulltext
Hydatid Disease (HD) is a serious public health problem in sheep and cattle raising countries like Australia, Africa, South America, Middle East and India. It is caused by the larval stage of Echinoccocus granulosus. It usually affects the liver (60-70%) and the lung (20-30%), but can develop anywhere in the body (5-10%) including the spleen, pancreas, kidney, peritoneum, retro-peritoneum, soft tissue, breast and central nervous system1.
Retroperitoneal hydatid cysts are usually secondary to spontaneous/traumatic rupture of liver hydatid cysts or surgical inoculation of liver hydatid cysts2. Primary isolated retroperitoneal hydatid cyst (PIRHC) without liver and lung involvement is extremely rare. We report herein a case of primary retroperitoneal hydatid cyst without any other organ involvement.
Case Report
A 45-year-old woman was admitted in our hospital with oneyear history of pain in the right lower quadrant of the abdomen. Six months earlier, she had noticed a lump in the right lower quadrant of abdomen. There were no complaints of altered bowel habits, fever, vomiting, jaundice or gastrointestinal bleed. She had a normal appetite and no history of weight loss. Her vital signs were normal. Systemic examination was normal. Local examination revealed a 15x10 cm non-tender lump in the right iliac fossa, which did not fall forward in knee-elbow position. Per vaginal and per-rectal examinations were normal.
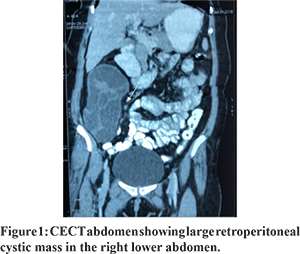
Blood investigations were within normal limits. Ultrasonography of the abdomen showed a 15x10 cm well-defined cystic lesion with thick sepations and multiple daughter cysts. The features were suggestive of a retroperitoneal hydatid cyst. Contrast enhanced Computerised Tomography (CECT) abdomen (Figure 1) showed a 15 x 9.5 cm large well defined, lobulated cystic lesion extending from the right sub-hepatic region to the right iliac fossa. The lesion had a multi-loculated appearance with numerous peripherally arranged daughter cysts. The lesion displaced the right kidney superiorly with alteration of the renal axis. The right hemi colonwas displaced anteriorly. The liver appeared normal. The findings were suggestive of a retroperitoneal hydatid cyst. Serological testing for hydatid disease (latex agglutination test) was negative. Based on clinical and imaging evidence, a provisional diagnosis of primary isolated retroperitoneal hydatid cyst was made and albendazole was started before surgery.
Exploratory laparotomy by midline incision revealed a large cystic mass in the right retroperitoneum, behind the right colon without any adhesion to the kidney, right colon, mesentery or major blood vessels (Figure 2). The liver appeared normal. Total excision of the cyst was done without perforation and spillage (Figure 3). The post-operative period was uneventful. Histopathology confirmed the diagnosis of hydatid disease. The patient was discharged on the 9th post-operative day on anthelmintic medication. At 3 months follow-up, the patient remained symptom-free with no radiological evidence of recurrence.
Discussion
Primary isolated retroperitoneal hydatid cysts (PIRHC) are extremely rare. The primary retroperitoneal hydatid cyst was first reported by Lockhart and Sapinza in 1958. The incidence of PIRHC is 0.5-2%3. The possible explanations for the formation of a PIRHC are embryosthe reaching systemic circulation after bypassing the liver and lungs, penetrating intestinal wall and enteringthe lymphatic system, through veno-venous shunts within the liver and in the space of Retzius. Some author had suggested airborne transmission and direct implantation of embryo in the bronchial mucosa, which then reaches the left heart to involve other sites4. However this remains largely hypothetical and needs to be proved. The differential diagnosis of retroperitoneal cystsinclude cystic lymphangioma, ovarian neoplasm, teratoma, retroperitoneal abscesses, soft tissue tumors, embryonal cysts and other cystic and necrotic tumors.
There are no specific local or general symptoms and signs of hydatid disease and it is often diagnosed as an incidental finding on radiological examination for unrelated symptoms. The most common symptoms of retroperitoneal hydatid cyst are abdominal pain and abdominal lump. Our case presented with both abdominal pain and lump. Some may present with complications such as rupture of retroperitoneal hydatid cyst into blood vessels, ureteric invasion, and pressure effects to adjacent structure or secondary infection of the cyst.
Routine blood tests are usually normal, but eosinophilia may be seen in 25% of cases5. Serological tests may be complimentary to the diagnosis. The sensitivity of IgG antibody by ELISA and indirect hemagglutination test are 95% and 87.5% respectively. Plain x-ray abdomen may reveal cyst wall calcifications. Ultrasonography is the investigation of choice for both hepatic and extra-hepatic hydatid cysts. It may show a well-defined anechoic mass with or without hydatid sand and septa, a dividing septa or daughter cysts within a fluid filled mass or a calcified cyst and undulating membranes. CECT abdomen may help in confirming the diagnosis. CT also provides information about the exact location of the extra-hepatic cyst and its relation to adjacent structures. Magnetic resonance imaging (MRI) typically shows the cyst to be of low intensity on T1-weighted scans and of high intensity on T2-weighted scans. The septa and cyst wall enhance after contrast administration and a low signal intensity rim on T2-weighted MRI is a characteristic finding of hydatidosis.
The treatment of primary extra-hepatic (retro-peritoneal) hydatid cyst depends on the size, site, symptoms and overall health status of the patient. Asymptomatic, small cysts can be treated with anti-helminthic drugs given for 3 weeks in one to eight repeating cycles with drug-free intervals of 2 to 3 weeks5. Surgery remains the best option for symptomatic and large cysts. The goals of hydatid cyst surgery are sterilisation of cyst contents, removal of all living cyst from the patient and complete excision of the germinal membrane. In our case, total hydatid cystectomy was performed without perforation/spillage and post-operative albendazole treatment was continued to prevent recurrence.
Conclusion
This case has been reportedto highlight the importanceof a high index of suspicion of hydatid disease in any retroperitoneal cyst in endemic areas. The definitive diagnosis may require cyst excision and histopathological examination of the resected specimen. Total cystectomy is the treatment of choice. Cyst deroofing and wide drainage can be done when complete excision is not possible due to dense adhesion to vital structures.
References
- Prousalidis J, Tzardinoglouk K, Katsokis C, Aletras C. Uncommon sites of hydatid disease. World J Surg 1998; 22:17-22.
- Sekar NN, Madhavan KK, Yadav RV, Katariya RN. Primary retroperitoneal hydatid Cyst(a report of 3 cases and review of the literature). J Postgrad Med ? 1982;28:112-4B
- Khwaunju P, Tamrakar KK, Sah K, Neupane HC: A case of primary retroperitoneal hydatid. Journal of Chitwan Medical College 2015; 5: 66-9
- Afak YS, Arif HS, Ajaz AM, Mubashir S et al. Primary Retroperitoneal Hydatid cyst: a Rare Case Report. Acta Med Iran 2015;53:448-451.?
- Karavias DD, Vagianos CE, Kakkos SK, et al. Peritoneal echinococcosis. World J Surg 1996;20:337-40.