48uep6bbphidcol2|ID
48uep6bbphidvals|2964
48uep6bbph|2000F98CTab_Articles|Fulltext
Immunoglobulin G4 (IgG4)-related disease is a systemic inflammatory syndrome characterized by obliterative phlebitis, fibrosis in the organs like pancreas, gallbladder, bile duct, salivary gland and extensive infiltration of IgG4-positive plasma cells and lymphocytes.1,2 The imaging findings are similar to those of a mass forming lesion. Thus, surgical resection is usually required even in cases where serum IgG levels are normal. Xanthogranulomatous change is a concurrent finding in some cases of IgG4 cholecystitis and should, thus be kept as a differential. We describe a case with overlapping features of IgG4 cholecystitis and xanthogranulomatous cholecystitis presenting as a diagnostic dilemma.
Case Report
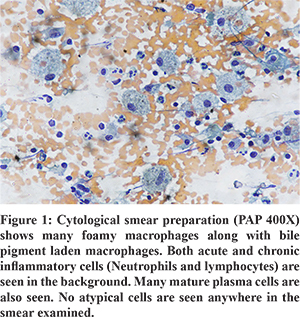
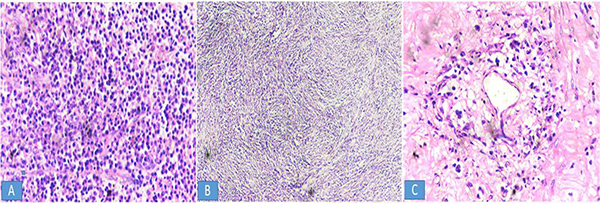
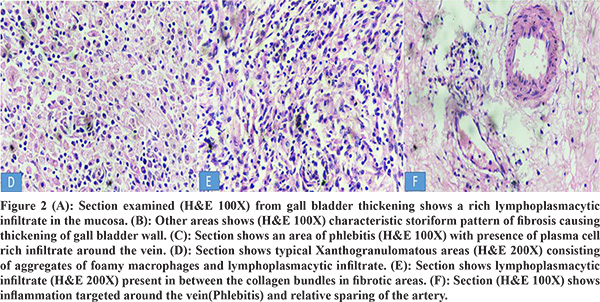
A 60-year-female visited hospital with complaints of pain in the right upper abdomen and intermittent fever for 3 months. On examination, there was tenderness and a hard globular well defined mass in the right upper quadrant. Preliminary investigations such as complete hemogram, liver function tests and kidney function tests were normal. Ultrasound whole abdomen revealed circumferential gall bladder wall thickening with an ill-defined hypoechoic lesion in the fundal region and an ill-defined hepatic fat plane. Contrast enhanced computed tomography (CECT) of the abdomen revealed a grossly distended gall bladder with asymmetric wall thickening and a 12 mm impacted calculus at neck along with pericholecystic fat stranding. CA 19.9 was raised. Exfoliative cytology from the gall bladder mass was suggestive of an inflammatory lesion; however, the possibility of a coexisting neoplasm could not be ruled out. (Figure 1) Cholecystectomy was performed. Gross pathological examination showed the gall bladder to be adherent to the liver bed with gall bladder wall thickening varying from 0.5 to 1.2 cm. The thickened wall showed irregular areas of fatty infiltration.Microscopic examination showed transmural diffuse lymphoplasmacytic infiltration and dense storiform fibrosis with focal areas showing perineural plasma cell infiltrate. Focal areas showed xanthogranulomatous inflammation comprising of foamy histiocytes along with obliterative phlebitis. (Figure 2) However, the accompanying arteries were unremarkable. No evidence of malignancy was seen. A differential diagnosis of xanthogranulomatous cholecystitis or Ig G4 related cholecystitis was kept on the basis of above findings. Immunohistochemical staining for IgG4 plasma cells was negative. As the histological findings were highly suggestive of IgG4-related disease, the patient was diagnosed as probable IgG4-related cholecystitis despite the absence of IgG4 staining and normal levels of serum IgG4.
Discussion
IgG4-related systemic disease is a multiorgan systemic fibroinflammatory disease but it can also present as an isolated lesion in a single organ. It may present synchronously or metachronously as tumefactive lesions or diffuse inflammatory lesioncausing pancreatitis, cholangitis, cholecystitis, sialadenitis, retroperitoneal fibrosis, inflammatory aortic aneurysm, or inflammatory pseudotumors. Serum IgG4 a subclass of IgG that is mostly elevated in this condition; however, some cases may show normal levels. Thus, it should be supported by additional histomorphological features along with immunohistochemical analysis. The pathognomonic features of IgG4 related disease on microscopic examina-tion are storiform fibrosis, a dense lymphoplasmacytic infiltrate with an increased number of IgG4+ plasma cells (at least > 10/high power field (HPF) – depending on the particular organ) and an obliterative phlebitis.3 Recently, a Japanese study group proposed a 3-tiered diagnostic terminology for IgG4-RD4. According to them the cases which either lack the full histological spectrum associated with IgG4-related disease or the immunohistochemical profile of IgG4-related disease should be labelled as probable histological features of IgG4-Related Disease. Inflammatory conditions like xanthogranulomatous cholecystitis may be confused with IgG4 cholecystitis due to overlapping histomorphological features like fibrosis, foamy histiocytes and lymphoplasmacytic infiltrate. Furthermore, the imaging findings in both these entities can appear similar to those of a malignant mass.5 Thus, histopathological examination is mandatory for differentiating these inflammatory lesions. In our case, histological features of xanthogranulomatous change like foamy histiocytes, lymphoplasmacytic infiltrate and fibrosis were noticed. However, the features favoring IgG4 cholecystitis were storiform fibrosis and obliterative phlebitis which are not seen in xanthogranulomatous cholecystitis. The case described above had a clinical presentation similar to that of a malignant mass and histological features of that of IgG4 related diseases with negative immunohistochemistry and serology, and was thus difficult to diagnose. IgG4 cholecystitis is usually seen in association with autoimmune pancreatitis. However, we present a case of isolated IgG4 cholecystitis without any association with autoimmune pancreatitis. To the best of our knowledge only one such case has been reported.5
Conclusion
Xanthogranulomatous cholecystitis and IgG4 Cholecystitis have overlapping features and can be confused on histomorphological diagnosis due to similar microscopic appearance. Thus, immunohistochemical and serological analysis for IgG4 positive cells should be done. However, cases which are negative for IgG4 on serology and immunohistochemistry but have a histopathologic picture resembling that of IgG4 disease may be labelled as probable IgG4 cholecystitis. Such cases need to be kept in follow up and evaluated radiologically and serologically for the propagation of disease to other organs.
References
- Finkelberg DL, Sahani D, Deshpande V et al. Autoimmune pancreatitis. N Engl J Med. 2006;21; 355: 2670-6.
- Kitagawa S, Zen Y, Harada K et al. Abundant IgG4-positive plasma cell infiltration characterizes chronicsclerosing sialadenitis (Küttner’s tumor). Am J Surg Pathol. 2005; 29: 783-91.
- Deshpande V, Zen Y, Chan JK et al. Consensusstatement on the pathology of IgG4-related disease. Mod Pathol. 2012; 25: 1181-92.
- Umehara H, Okazaki K, Masaki Yet al. Research Program for Intractable Disease by Ministry of Health, Labor and Welfare (MHLW) Japan G4 team. A novel clinical entity, IgG4-related disease(IgG4RD): general concept and details. Mod Rheumatol. 2012; 22: 1-14.
- Hong SA, Sung YN, Kim HJ et al. Xanthogranulomatous cholecystitis shows overlapping histologicalfeatures with IgG4-related cholecystitis. Histopathology. 2018; 72:569-579.