Cystic fibrosis (CF; OMIM: 219700), is an autosomal recessive disease caused by the homozygous or compound heterozygous mutations of the cystic fibrosis transmembrane conductance regulator (CFTR) gene (OMIM*602421) encoding the CFTR protein. It is the most common lethal genetic disease among Caucasians, with a reported birth prevalence of 1:2000-1:4000 live births. The CFTR dysfunction affects epithelial cells, compromising innate and adaptive immune systems both in terms of quality and quantity of response resulting in immunological imbalance; which provides the basis for developing autoimmune diseases (AID) as comorbid conditions. In CF, the most investigated AID is celiac disease.1
The risk of the co-morbidity of CF and CD has also been suggested previously. The incidence of the two conditions occurring in the same patient has been estimated to be 1 in 2,000,000-1:5,900,000. Several case–control studies reporting a wide range (1.2-2.13%) of proven CD incidence in European CF patients have been published in the last decade2.
We report a case in which the female child was diagnosed with this co-morbidity at 14 years of age. We conclude that despite the different pathophysiology, both CF and CD cause malabsorption; and pose a diagnostic dilemma for pediatricians in distinguishing between CF-related or potentially CD-related GI symptoms. A better understanding of the comorbidity of both diseases is needed for early diagnosis and management.
Case Report
A 14 Years old female child, known patient of celiac disease for the last 10 years; on a gluten-free diet, presented with complaints of recurrent respiratory infections, undocumented fever in the last year and cough in the last 6 months. Fever had a diurnal variation with evening rise of temperature and was aggravated in the last 20 days. Cough was mucoid, greenish-colored, non-blood stained, and associated with respiratory difficulty and fever. She also has a history of oily stools, constipation and failure to gain weight. The patient kept on taking medications from various pediatricians with symptomatic relief only.
She was hospitalized at 3 years of age for cough and respiratory distress at 4 years of age with complaints of constipation and surgery for bowel obstruction, and at 7 years of age for cough, fever and blood transfusion. Her mother’s younger sister was also diagnosed with celiac disease. Her antenatal course was uneventful but there was history of meconium-stained liquor. She was given mixed feeding and weaning was started at 7 months. She is incompletely immunized. Currently, she is taking milk, makhane, cornflakes, 2 chapatis of celiac flour, vegetables, dal and tea.
On examination, her height was 138 cm which was < 3rd centile and her weight was 23 kg which was also < 3rd centile for age. Her body mass index (BMI) was also < 3rd centile. Digital clubbing on both hands and right nasal polyp with inferior turbinate hypertrophy was noted, and nasal mucosa was pink. The tongue was pink and dental hygiene was adequate. Respiratory system examination revealed symmetric bilateral chest movements and expansion with no visible scars or swelling. Trachea was midline. Air entry was equal with resonant bilateral lungs. Coarse crepitations were present on both sides. Abdomen was scaphoid and all quadrants moved equally with respiration. A scar of 6x1 cm was present on the right lumbar region. No visible veins were noted. The abdomen was soft and bowel sounds were audible. No hepatosplenomegaly was noted.
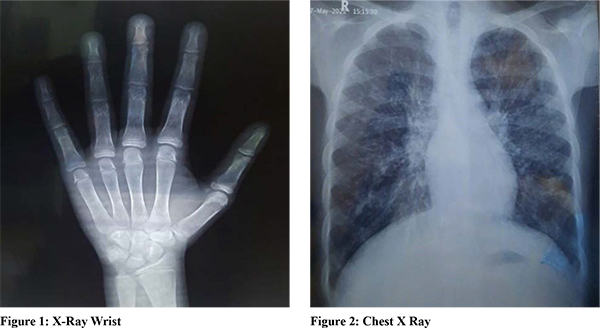
Her complete blood counts were normal with slight leukocytosis of 11.12 x 103/µl, with normal differential counts. Hemoglobin was 12.9 gm/dl with normal MCV, MCH and MCHC and normal platelet counts. Investigations have been summarized in Table-1 and Figure 1,2. Sputum for AFB and CBNAAT were negative. The diagnosis of celiac disease was confirmed by upper GI endoscopy and duodenal biopsy (modified Marsh Type 2). Positive HLA DQ2.5 endorsed the diagnosis.


CECT Scan of the thorax revealed multiple centrilobular nodules (tree-in bud pattern) in the anterior segment of the bilateral upper lobe, the lateral segment of the right middle lobe, the anterior-basal segment, the lateral-basal segment of the right lower lobe, lingula of left upper lobe, the superior-basal, antero-medial-basal and lateral basal segment of left lower lobe. Patchy ground glass haziness was noted in the anterior segment of the left upper lobe and the posterior basal segment of the left lower lobe. Bronchial wall thickening was noted in the bilateral lung parenchyma. No evidence of enlarged lymph nodes was seen in the mediastinum and hilar regions. Overall findings were suggestive of bronchial wall thickening with centrilobular nodules and ground glass haziness consistent with infective bronchiolitis.
MRI of abdomen and pelvis with gadolinium (Tech: SE TI & FSE -T2 weighted axial & Coronal images of the upper abdomen along with axial T 1, T2 and coronal FSIR & sag T2W images of the lower abdomen); revealed a fibrotic pancreas and both ovaries had antral follicles arranged peripherally giving a necklace-like appearance, with thickened stroma suggestive of polycystic ovarian disease (PCOD). The uterus was very small in size. Rest of the intraabdominal organis were normal (Figure-3).
Tests for the exocrine pancreatic function showed decreased insulin and C-peptide levels but no hyperglycemia was documented or reported. Immunoreactive trypsinogen for the immunoreactive trypsinogen was reported as negative.
Whole Exome sequencing detected likely pathogenic variant causative of the reported phenotype (Table 3). A homozygous start loss variation (that alters the ATG start codon and consequently affects its translation) in exon 1 of the CFTR gene (chr7: g.117480096T>C; Depth:104x) (p.Met 17; ENST00000000-3084,11) was detected. The observed variant has previously been reported as p. MIT in patients with cystic fibrosis. The p. Met1 (suspected) variant has not been reported in the 1000 genomes and genome databases and had a minor allele frequency of 0.015% in concerned internal database. The in-silico prediction of the variant damages by SIFT, LRT, and mutation Taster 2. The reference codon is conserved across species. The child was given protocol management with a gluten-free diet and nutritional counselling. She got improved and was discharged with the advice of chest physiotherapy and education for symptoms of pulmonary exacerbation.
Discussion
Cystic fibrosis is characterized by a triad of chronic obstructive pulmonary disease, exocrine pancreatic insufficiency, and elevation of sodium and chloride concentration in sweat. Immune dysregulation in CF is hypothesized to be due to lipopolysaccharide hypersensitivity of alveolar macrophages; enhanced signal transduction via NF-?B and MAPK pathways; altered LPS-induced metabolic pathways; impaired apoptosis of granulocytes; and an increased release of various proinflammatory cytokines, including IL-17 and IL-6, etc.2-5.
The child in our case report was on a gluten-free diet and was well conversant with the importance of a GFD. Despite a better understanding of the course, nature and prognosis of disease; the child didn’t grow well and suffered recurrent illnesses and could only be diagnosed to have co-morbidity of cystic fibrosis at a later age. The heavy burden of undigested gluten proteins in the intestine due to exocrine pancreatic insufficiency, intestinal mucosal damage due to malnutrition and an immunological response against wheat gluten may explain her condition.
Conclusion
Clinical symptoms and signs of CD are difficult to differentiate from CF with malabsorption, and we, therefore, suggest that serological screening for CD should be included in the diagnostic work-up of CF patients older than nine months and patients with persistent gastrointestinal symptoms. Such case reports suggest the importance of screening for CD in CF and vice versa. Further studies should be undertaken for the estimation of the prevalence of CF in Indian CD children. The clinical phenotype of CF with and without CD should be described in detail to define those who might benefit from CD screening and, later, from the gluten-free diet.
References
- Castellani, C.; Duff, A.J.; Bell, S.; Heijerman, H.G.; Munck, A.; Ratjen, F.; Sermet-Gaudelus, I.; Southern, K.W.; Barben, J.; Flume, P.A.; et al. ECFS best practice guidelines: The 2018 revision. J. Cyst. Fibros. 2018, 17, 153–178
- Lahiri, T.; Hempstead, S.E.; Brady, C.; Cannon, C.; Clark, K.; Condren, M.E.; Guill, M.F.; Guillerman, R.P.; Leone, C.G.; Maguiness, K.; et al. Clinical Practice Guidelines from the Cystic Fibrosis Foundation for Preschoolers with Cystic Fibrosis. Pediatrics 2016, 137, e20151784.
- Al-Toma, A.; Volta, U.; Auricchio, R.; Castillejo, G.; Sanders, D.S.; Cellier, C.; Mulder, C.J.; Lundin, K.E.A. European Society for the Study of Coeliac Disease (ESsCD) guideline for coeliac disease and other gluten-related disorders. United Eur. Gastroenterol. J. 2019, 7, 583–613.
- Husby, S.; Koletzko, S.; Korponay-Szabó, I.; Kurppa, K.; Mearin, M.L.; Ribes-Koninckx, C.; Shamir, R.; Troncone, R.; Auricchio, R.; Castillejo, G.; et al. European Society Paediatric Gastroenterology, Hepatology and Nutrition Guidelines for Diagnosing Coeliac Disease 2020. J. Pediatr. Gastroenterol. Nutr. 2020, 70, 141–156.
- Imrei, M.; Németh, D.; Szakács, Z.; Hegyi, P.; Kiss, S.; Alizadeh, H.; Dembrovszky, F.; Pázmány, P.; Bajor, J.; Párniczky, A. Increased Prevalence of Celiac Disease in Patients with Cystic Fibrosis: A Systematic Review and Meta-Analysis. J. Pers. Med. 2021, 11, 859.