|
Sudhir Maharshi, Dilip Singh Mudgal, Shyam Sunder Sharma, Kamlesh Kumar Sharma, Bharat Sapra, Rupesh Pokharna, Sandeep Nijhawan Department of Gastroenterology, SMS Medical College and Hospitals, Jaipur, India.
Corresponding Author:
Dr. Sudhir Maharshi Email: sudhir.maharshi@gmail.com
Abstract
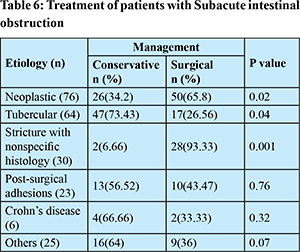
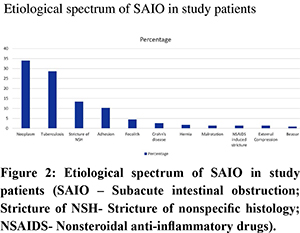
Background: Regional as well as worldwide variations in the pattern of sub-acute intestinal obstruction (SAIO) from time to time are well documented, but most of these studies are from surgical departments.There is a lack of data on etiological spectrum of SAIO in patients who are consulting in gastroenterology department. Aims: The aim was to study the etiological, clinical profile and treatment outcomesof SAIO patients who were presented to gastroenterology department. Methods: This prospective descriptive study was conducted in the department of gastroenterology,SMS medical college and hospitals, Jaipur between August 2019 to July 2021. All the patients with clinical diagnosis of SAIO were consecutively enrolled. Data related to demography, clinical features, laboratory parameters, radiological imaging, histology and treatment outcomes were analyzed. Results: A total of 224 patients (age 43.7±13.7 years, BMI 17.1±3.1kg/m2, 57.14% male) were studied. Etiology of SAIO was neoplastic 76(33.92%), tuberculosis 64(28.57%), benign stricture with non-specific histology 30(13.39%) and adhesions in 23(10.27%) patients. Surgical treatment was required more in neoplastic (65.8% vs 34.2%; p=0.02) and benign stricture with non-specific histology (93.33% vs 6.66%; p=0.001) while conservative treatment including antitubercular therapy and endoscopic dilatations if required was more successful in tubercular etiology (73.43% vs 26.57%, P=0.04). Conclusion: Neoplasm is the most common cause of SAIO in gastroenterology practice, followed by tubercular, benign stricture with non-specific histology and adhesions. Majority of tubercular patients can be treated with conservative treatment while surgical management is needed more in neoplastic and benign stricture with non-specific histology.
|
Introduction
Intestinal obstruction is defined as decreased passage of intestinal contents, which may be either due to mechanical obstruction (dynamic) or due to absent/reduced intestinal motility in the absence of obstructing lesion.1 Intestinal obstruction is the most common surgical disease of small intestine and is associated with significant morbidity and mortality.2,3 The diagnosis of intestinal obstruction is usually easy but it is difficult in patients with sub-acute intestinal obstruction (SAIO). These patients may present with atypical signs and symptoms that causes delay in diagnosis and may continue to suffer for weeks to months. Sub-acute intestinal obstruction is defined as incomplete, intermittent or recurrent obstruction.4,5 It is manifested by continued passage of flatus and/or stools beyond 6-12 hours after the onset of clinical features like colicky abdominal pain, vomiting and abdominal distension.3 It may present as acute intestinal obstruction and the patient may improve either spontaneously or after conservative treatment within 6-12 hours. The etiology of intestinal obstruction can be classified into three categories, first, obstruction originating from extra-luminal causes like adhesion, neoplasm and hernia. Second, obstruction intrinsic to intestinal wall such as primary neoplasm and third, intra-luminal obstruction like gall stones, enterolith, bezoars and foreign bodies.6 Appropriate history, clinical examination and imaging helps in the diagnosis of SAIO. For etiological evaluation, patient is usually subjected to special investigations like upper gastrointestinal endoscopy, enteroscopy, colonoscopy with biopsy and in patient of unresolved obstruction, laparotomy discovers the cause in most of the cases.7 There are few studies on etiological, clinical and pathological profile of SAIO patients but most of these studies are published from surgical departments where chances of undergoing surgical treatment are more.6,8 There is paucity of data on patients of SAIO, primarily presenting to gastroenterology departments. So, this study aimed to assess the etiological, clinical profile and treatment outcomes of SAIO patients who presented to the gastroenterology department. Methods
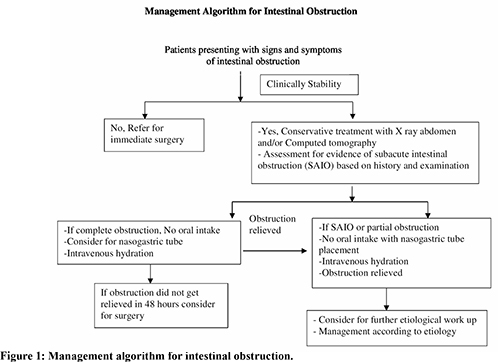
This prospective descriptive study was conducted in the department of gastroenterology at SMS Hospital, Jaipur, Rajasthan, India from August 2019 to July 2021. Informed consent in writing was obtained from each patient and the study protocol confirmed to the ethical guidelines of the 2000 declaration of Helsinki as reflected in priori approved by the appropriate institutional ethics committee (Ethics committee number 3981 MC/EC/2018). Inclusion criteria were patients of age more than 18 years presenting with features of intestinal obstruction with passage of flatus and/or stools beyond 12 hours of the onset of symptoms, a lesser degree of abdominal distension, gas distended intestinal loops and/or multiple air-fluid levels on imaging. Patients presenting with acute obstruction and/or with features of strangulation, paralytic ileus, pseudo-obstruction and anorectal malformation were excluded from the study.After admission a detailed history was taken followed by clinical examination. Laboratory investigations including hemogram, erythrocyte sedimentation rate (ESR), liver function test, kidney function test, electrolytes and acid base analysis along with plain radiograph of abdomen were done. Study patients were started on conservative treatment including nil per oral, nasogastric tube insertion with continuous lavage, intravenous antibiotics (ceftriaxone + metronidazole) along with fluids, analgesics and antiemetics. Patients who were relieved from the obstruction underwent further etiological work up including chest radiograph, ultra-sonography (USG) abdomen, contrast enhanced computed tomography (CECT) scan, upper gastrointestinal endoscopy and/or enteroscopy and/or colonoscopy with biopsy and diagnostic laparoscopy as required. Mantoux test was considered in patients where tuberculosis was clinically suspected. When the obstruction did not relieve within 48 hours of conservative treatment, patients were referred to the surgical department. The management algorithm followed for intestinal obstruction is shown in Figure 1. Patients of neoplastic etiology were referred to surgical and oncology departments for further management. Intestinal tuberculosis was diagnosed on the basis of pathological findings in small and/or large intestine revealing acid-fast bacilli (AFB) on Ziehl Neilson staining or polymerase chain reaction (PCR) positivity for Mycobacterium tuberculosis on endoscopic biopsies. The presence of epithelioid granulomas, along with unequivocal clinical response to 6-8 weeks anti-tubercular therapy (ATT), were also taken as diagnostic criteria for intestinal tuberculosis, whenever AFB could not be reported. Patients with tuberculosis received four drug ATT (rifampicin, isoniazid, pyrazinamide and ethambutol) in proper doses in intensive phase followed by rifampicin, isoniazid and ethambutol in the continuation phase. All the patients were followed up for 6 months to assess the treatment outcome. Patients of tubercular terminal ileal stricture symptomatic, inspite of taking ATT, underwent endoscopic balloon dilatation through the scope (TTS) balloon (Wilson Cook, NC USA). Serial dilatation was done at an interval of 2 weeks starting with balloon size of 12 mm. The end point of dilatation was arbitrarily defined as successful dilatation with 16 mm balloon with amelioration of clinical symptoms. All the patients who underwent dilatations were admitted for observation and monitoring. Data related to etiology, clinical profile and treatment outcomes were analyzed.
Statistical Analysis
The statistical analysis was performed using statistical package for social sciences (SPSS) version 22.0 for Windows (SPSS, Chicago IL, U.S.A). Data were expressed as absolute number and percentage for categorical variables and mean ± standard deviation (SD) or median and ranges were calculated for continuous variables as appropriate. Non-parametric test, Wilcoxon’s sign rank test and Mann Whitney U test were used to compare the difference in mean/median value of paired and unpaired data respectively. Multivariate logistic regression analysis used to perform multivariate analysis. A p value of < 0.05 was considered to be significant.
Result
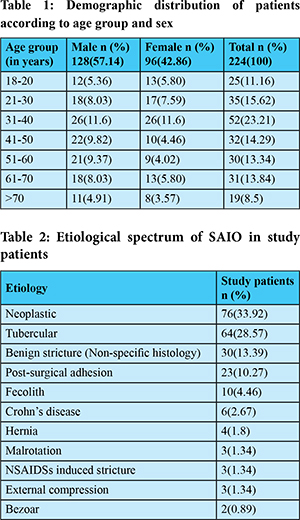
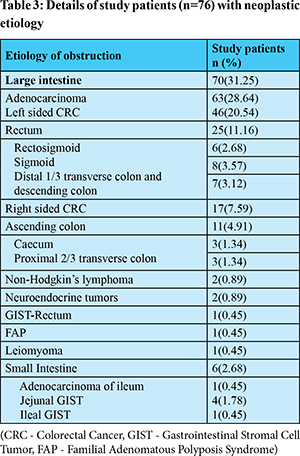
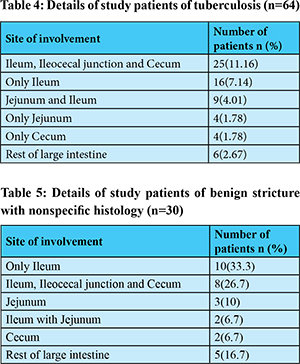
A total of 224 SAIO patients (age 43.7±13.7 years, BMI 17.1±3.1kg/m2) were studied during the study period.The most common affected age group was 31-40 years with 23.21% patients followed by 21-30 years group with 15.62% patients. Males 128 (57.14%) were more commonly affected compared to females 96 (42.86%) as shown in Table 1. The small intestine 128 (57.14%) was more commonly involved than large intestine 96 (42.86%). The most common presenting symptom was colicky abdominal pain 210 (93.75%) followed by vomiting 178 (79.46%), constipation and/or obstipation 138 (61.60%) and abdominal distension in 108 (48.21%) patients.The signs observed in the study patients include exaggerated bowel sounds in 152 (67.85%) patients and visible peristalsis in 54 (24.10%). Majority 138 (61.6%) of patients presented within 2-5 days, 40 (17.86%) within one day, 35 (15.62%) within 6-7 days while 11 (4.9%) patients presented after 7 days of symptom onset. First obstructive attack of SAIO was observed in 110 (49.10%) patients, second in 41(18.3%), third in 34 (15.17%), fourth in 21 (9.37%) while 18 (8.03%) patients had five or more attacks. Intestinal neoplasm 76 (33.95%) was the most common cause followed by intestinal tuberculosis 64 (28.57%), stricture of non-specific histology 30 (13.39%) and post-surgical adhesions 23 (10.27%). Complete etiological spectrum of study patients is shown in Table 2 and Figure 2. Neoplasms were more common in large intestine70 (92.11%) compare to small intestine 6 (7.89%). In large intestine, adenocarcinoma (90%) was the most common neoplasm while in small intestine jejunal gastrointestinal stromal cell tumor (GIST) was more common (66.66%). Large intestinal adenocarcinoma was more common in left side colon (73.01%) compared to right side colon (26.98%). The details of neoplastic etiology is described in Table 3. Out of 64 patients of tuberculosis only 10 patients had acid-fast bacilli (AFB) on Ziehl Neilson staining or polymerase chain reaction (PCR) positivity for Mycobacterium tuberculosis on endoscopic biopsies. The remaining 54 patients had epithelioid granulomas with chronic inflammatory cells, along with unequivocal clinical response to 6-8 weeks anti-tubercular therapy (ATT) and none of the patient had started on empirical treatment without diagnosis. Intestinal tuberculosis involving ileum, ileocecal junction along with caecum was most common (39.06%) compared to other sites as described in Table 4. Associated pulmonary tuberculosis was observed in 11 (17.18%) patients. Only Ileum (33.33%) was most common site for strictures with non-specific histology followed by at ileum, ileocecal junction along with caecum involvement 26.7% as shown in Table 5. These patients underwent CECT abdomen with enterography, ileo-colonoscopy with multiple biopsies for further evaluation to establish their etiology, but inspite of extensive evaluation their etiology could not be established and they were classified as strictures with non-specific histology. None of these patients had past history of tuberculosis.Thirty-four (15.17%) patients had past history of abdominal surgery. The causes for previous abdominal surgery were intestinal obstruction or perforation (12), abdominal trauma (8), gynecological surgery (5), hernia repair (3), appendicectomy (3) and it was not known in 3 patients. Surgical treatment was required in 116 (51.8%), while 108 (48.2%) patients were treated conservatively. Out of 116 patients who underwent surgery, 68 (30.35%) underwent emergency surgery as they did not respond to conservative treatment.The remaining 156 (69.64%) patients did not require emergency surgery and their obstruction relieved within 48 hours of admission. On further evaluation etiology was identified required elective surgical management in 48 (21.4%) patients. The details of management of study patients including conservative and surgical has been shown in Table 6. Need of surgical treatment was more in patients of neoplastic (65.8% vs 34.2%; p=0.02) and stricture with non-specific histology (93.33% vs 6.66%; p=0.001) while in patients of tuberculosis, at the end of 6 months follow up, conservative treatment was more successful (73.43% vs 26.56%; p=0.04). The most common surgical management offered to neoplastic patients was hemicolectomy with anastomosis depending on the site of lesion. Among the neoplastic etiology 26 patients were unresectable and/or unfit for the surgical treatment. These patients were treated with chemotherapy along with palliative treatment. Colonic self-expandable metallic stent (SEMS) was placed in 5 patients with rectosigmoid malignancies. Eight (12.5%) patients with terminal ileal tubercular stricture and one patient of benign stricture with nonspecific histology underwent endoscopic dilatation with median of 2 (range 1-3).The mean follow-up period for stricture of benign etiology was 6.6±3.2 months and during this follow up 38 (25.6%) patients developed recurrence of symptoms. On multivariate logistic regression analysis only duration of symptom onset [Odds ratio (OR) 2.145, 95% confidence interval (CI) 1.582-2.836, P=0.01], etiology (OR 1.786, 95% CI 1.318-2.382, p=0.02) and age <40years (OR 1.684, 95% CI 1.314- 2.168, p= 0.04) were independent predictors for response to conservative treatment.
Discussion
Sub-acute intestinal obstruction is a common surgical disorder. Its diagnosis is usually delayed and many patients suffer from symptoms for long duration. It affects both small and large intestine. Most of the published literature on acute intestinal obstruction and SAIO patients is from surgical departments. Patients with SAIO are also commonly seen and managed in gastroenterology departments. In view of lack of data on SAIO from gastroenterology practices we conducted this study in our department. In our study the most common affected age group was 21-40 years, similar to previously published studies.6,7,9-12 However, in few studies the most common affected age group was >40 years.8,13-15 In our study, males 128 (57.14%) were more common compared to females 96 (42.86%) in concordance to previous studies.6,7 Our study revealed that small intestine 128 (57.14%) was more commonly affected compared to large intestine 96 (42.86%), these results are in agreement with previously published studies.9,10,12-14,16-18 In another study large intestine was more commonly affected compared to small intestine.19 The most common presenting features in our study patients was abdominal pain followed by vomiting, exaggerated bowel sounds, constipation and/or obstipation, abdominal distention and visible peristalsis. Similar results were observed in previous studies.6,7 Majority of our patients presented between 2-5 days of symptom onset which is consistent with previous studies.9,10,12-14,16-18 In our study first obstructive attack of SAIO was observed in 110 (49.10%) patients while 18 (8.03%) patients had five or more attacks, similarly first obstructive attack was observed in 43% and 52.4% patients other two studies.6,7 Intestinal neoplasm 76 (33.95%) was the most common etiology in our study patients followed by intestinal tuberculosis 64 (28.57%), stricture of non-specific histology 30 (13.39%) and post-surgical adhesions 23 (10.27%). In various other studies adhesion has been considered as most important cause of intestinal obstruction and was observed in 45-80% of patients, but most of these studies were published from surgical departments and also included patients of acute intestinal obstruction.20-24 A previous study on SAIO patients also revealed adhesion (31.8%) and small bowel stricture (27.2%) as most common causes.7 Another study documented adhesion (36.2%) and intestinal tuberculosis (27.5%) as most common causes for SAIO.8 The probable reason of change in etiology in our study patients is likely due to study conducted in gastroenterology department on patients with SAIO and in 96 (42.86%) of study patients the etiology was in large intestine where neoplasm is common cause for SAIO. Another reason may be due to follow up of post-surgical and hernia patients in surgical outdoors, so these patients less commonly seen in gastroenterology outdoors. The higher contribution of neoplasm and tuberculosis in our study is also likely due to increasing incidence of malignancy in general population and high incidence and prevalence of tuberculosis in Indian population. Patients with neoplasm and tuberculosis usually also have associated clinical features like anorexia, weight loss, bleeding per rectum, malena, diarrhea, constipation, and fever. Due to these associated clinical features, such patients have more probability of attending gastroenterology outdoors compared to surgical outdoors. In other previously published studies on patients with intestinal obstruction neoplastic etiology was observed in 6-21% patients and in these studies, left side colonic adenocarcinoma was more common than right side as observed in our study.13,15,16,25-27 Colorectal cancer in India occurs one decade earlier than western population and the incidence rates for rectal cancer is higher than colon cancer in all parts of India.28 In this study the tubercular etiology observed in 64 (28.57%) patients. The tubercular etiology in previous studies on intestinal obstruction varies from 3.8% to 29%9,10,12-14,16-18 Our results are in agreement with two studies, which revealed tubercular etiology in 25% and 29% patients.12,18 Ileum, ileocecal junction along with caecum was most common (39.06%) site for intestinal tuberculosis, possibly because of the increased physiological stasis, increased rate of fluid and electrolyte absorption, minimal digestive activity and an abundance of lymphoid tissue at this site. Similarly, in other studies also tubercular ileocecal involvement observed in 36-54% of study patients.7,29-31 While in two studies most common site of involvement was small bowel in 42.42% and 56.55% patients instead of ileocecal region.32,33 In our study the chest x-ray changes suggestive of old healed or active pulmonary tuberculosis were observed in 17.4% of intestinal tuberculosis cases, similar results were seen in another study from India in which 25% cases had associated pulmonary tuberculosis.30 In other two studies the cases of associated pulmonary tuberculosis were high (39% and 46%).31,34 In our study benign stricture with nonspecific histology observed in 30 (13.39%) patients. In other studies, benign inflammatory stricture observed in 3.33%-30% patients.12,17-19 In our patients, conservative treatment resulted in relief of obstruction in 156 (69.64%) patients and unsuccessful in 68 (30.35%) patients. In other previously published studies, the success rate of conservative treatments was 34-73%.7,20,21,35-37 Need of surgical treatment was more in patients of neoplastic and stricture with nonspecific histology patients while in patients of other etiology conservative treatment was more successful. These results are similar to a previous study in which the need of surgery was observed in 86.7% patients of SAIO with malignant etiology.8 Majority (73.43%) of our intestinal tuberculosis patients were managed conservatively.Similarly, in another study 60.2% patients were managed conservatively.8 We described the detail etiological, clinical profile and treatment outcomesof SAIO patients presenting to gastroenterology department as there is limited data on it. Our study has few limitations,first, short duration of follow up in study patients. Second, we did not assess the role of investigations in the diagnosis of SAIO. Third, this etiological spectrum was limited to a tertiary referral centre. In conclusion neoplasm is the most common cause of SAIO in patients presenting to gastroenterology department, followed by tubercular, benign stricture with nonspecific histology and adhesion. Majority of tubercular patients can be treated with ATT and endoscopic dilatations if required while surgical management is more needed in neoplastic and benign stricture with non-specific histology. Further studies with long duration of follow up for assessment of predictors for success of conservative treatment is required.
References - Mizell JS, Turnage RH.Intestinal obstruction. In: Feldman M, Friedman LS, Brandt LJ editors.Sleisenger&Fordtran’s Gastrointestinal and liver disease: Pathophysiology/Diagnosis/Management. 10th ed. Philadelphia: Saunders; 2016.pp. 2154-70.
- Shelton AA, Thoedore RS, Welton ML.Small Intestine. In: Way LW, Doherty GM, editors.Current Surgical Diagnosis and Treatment. New York: McGraw Hills; 2003.pp. 674-704.
- Whang EE, Zinner MJ.Small Intestine. In: Charles BF editor.Schwartz principles of surgery. New York: McGraw Hill; 2005. Pp. 1017-54.
- Ahmed MN, Kaur SS, Zargar HU. Abdominal cocoon: an unusual cause of intestinal obstruction (a case report).Journal of Postgraduate Medicine.1984;30:62-3.
- Winslet MC. Intestinal Obstruction. In: Russel RCG, Norman WS, Bulstrode Christopher JK, editors.Bailey & Love’s Short Practice of Surgery. London: Arnold, 2004. pp.1186–202.
- Ojha A, Jalaj A, Tiwari S, Mujalde V, Prasheel. Diagnosis and management of subacute intestinal obstruction: a prospective study. Journal of Evolution of Medical and Dental Sciences.2014;3:7326-40.
- Jain BK, Agrawal J, Rathi V, Garg PK, Dubey IB. Subacute intestinal obstruction: an enigma revisited. Trop Doct. 2013;43:5-8.
- Sethi S, Raja Rajan BN. Subacute intestinal obstruction: an experience in eastern India. SAS Journal Surgery. 2017;3:214-7.
- Qureshi NA, Bhat SK, Sodhi BS. Spectrum of Etiology of Intestinal Obstruction - A Hospital-based Study. International Journal of Scientific Study.2017;5:85-9.
- Jaiswal NK, Shekhar S, Ranade P. Study of clinical spectrum and management of acute intestinal obstruction. International Surgery Journal.2018;5:1310-4.
- ArunKatari. A clinical study of acute intestinal obstruction in a tertiary care hospital of Telangana. Saudi Journal of Medicine.2018;3:482-6.
- Shukla S, Kumar K, Khusram B, Damor M. Clinico-pathological study of intestinal obstruction and its management. International Surgery Journal.2017;4:604-11.
- Pillai V, Benjamin RK, Chisthi MM. A Pattern of Intestinal Obstruction Cases – A Tertiary Care Centre Study. Annals of International Medical and Dental Research. 2017; 3:41-5.
- Mohamed A, Sahoo N, Das SK, Das BB, Pradhan SK, Gouda PK. Profile of operated acute intestinal obstruction patients at a tertiary health care institution. Journal of Evolution of Medical and Dental Sciences. 2017;6:1215-9.
- Jiang W,Li W, Hao Q, Yao Y, Li Y, Ge J, et al. Etiologic Spectrum of Intestinal Obstruction in Ningxia District: A Retrospective Analysis of 4908 Cases in a 10 Year Period. Gastroenterol Res Pract. 2019;26:4935947.
- Adhikari S, Hossein MZ, Das A, Mitra N, Ray U. Etiology and outcome of acute intestinal obstruction: A review of 367 patients in Eastern India. Saudi J Gastroenterol.2010;16:285-7.
- Tiwari SJ, Mulmule R, Bijwe VN. A clinical study of acute intestinal obstruction in adults-based on etiology, severity indicators and surgical outcome. International Journal of Research in Medical Sciences.2017;5:3688-96.
- Malik AM, Shah M, Pathan R, Sufi K. Pattern of Acute Intestinal Obstruction: Is there a change in the underlying etiology?. Saudi J Gastroenterol. 2010:16:272–4.
- Ullah S, Khan M, Mumtaz N, Naseer A. Intestinal obstruction: A spectrum of causes. Journal of Postgraduate Medicine.2009;23:186-92.
- Jr PM. Small intestinal obstruction. SurgClin North Am.1987;67:597-620.
- Cox MR, Gunn IF, Eastman MC, Hunt RF, Heinz AW. The operative aetiology and types of adhesions causing small bowelobstruction. Aust N Z J Surg.1993;63:848-52.
- Ellis H. The causes and prevention of intestinal adhesions. Br J Surg.1982;69:241-3.
- Menzies D, Ellis H. Intestinal obstruction from adhesions - how big is the problem? Ann R Coll Surg Engl.1990;72:60-3.
- Bizer LS, Liebling RW, Delany HM, Gliedman ML. Small bowel obstruction: the role of non-operative treatment in simple intestinal obstruction and predictive criteria for strangulation obstruction. Surgery.1981;89:407-13.
- Ojo EO, Ihezue CH, Sule AZ, Ismaila OB, Dauda AM, Adejumo AA.Aetiology, clinical pattern and outcome of adult intestinal obstruction in Jos, North Central Nigeria.AfrJMed MedSci. 2014;43:29-36.
- Peedikayil MC, Nair P, Seena SM, Radhakrishnan L, Sadasivan S, Narayanan VA, et al. Colorectal cancer distribution in 220 Indian patients undergoing colonoscopy. Indian J Gastroenterol.2009;28:212-5.
- Waheed DA, Ahmed DS,Ahmed SO, Bashir WS,Hanifa A,Subiya K, et al. Demographic profile of cancer colorectal and anal canal,a study conducted government medical college Srinagar Kashmir India A retrospective study. International Journal of Surgery Sciences. 2019;3:354-7.
- Rastogi T, Devesa S, Mangtani P, Mathew A, Cooper N, Kao R, et al. Cancer incidence rates among South Asians in four geographic regions: India, Singapore, UK and US. Int J Epidemiol.2008;37:147-60.
- Bhansali SK. Abdominal tuberculosis. Experiences with 300 cases.Am J Gastroenterol.1977 ;67:324-37.
- Tandon HD, Prakash A. Pathology of intestinal tuberculosis and its distinction from Crohn’s disease. Gut. 1972;13:260-9.
- Prakash A. Ulcero-constrictive tuberculosis of the bowel. Int Surg. 1978;63:23-9.
- Vij JC, Malhotra V, Choudhary V, Jain NK, Prasad G, Choudhary A, et al. Clinocopathological study of abdominal tuberculosis. Indian Journal of Tuberculosis.1992;39:213-20.
- Singh V, Jain AK, Agrawal AK, Gupta S, Khanna S, Khanna AK, et al. Clinicopathological profile of abdominal tuberculosis. Br J ClinPract.1995;49:22-4.
- Sharma MP, Bhatia V. Abdominal tuberculosis.Indian J Med Res. 2004;120:305-15.
- Miller G, Boman J, Shrier I, Gordon PH. Natural history of patients with adhesive small bowel obstruction. Br J Surgery.2000;87:1240-7.
- Tanphiphat C, Chittmittraprap S, Prasopsunti K. Adhesive small bowel obstructions. A review of 321 cases in a Thai hospital.Am J Surg.1987;154:283-7.
- Seror D, Feigin E, Szold A, Allweis TM, Carmon M, Nissan S, et al. How conservatively can postoperative small bowel obstruction be treated? Am J Surg.1993;165:121-6.
|