48uep6bbphidvals|375
48uep6bbph|2000F98CTab_Articles|Fulltext
Introduction
In 1881, Wolfer performed the first gastro-enterostomy, and approximately thirty-five years later in 1914, Bozzi described first case of jejunogastric intussusception (JGI) as its complication.[1,2] An estimated 0.1% of patients who have undergone Billroth II or Roux-en-Y reconstruction will develop intussusception.[3] Only around 200 cases of JGI have been reported in the literature till now.4 We report two cases of acute JGI, as they illustrate that upper GI endoscopy provides a quick, accurate diagnosis of this unusual condition and that early surgery can reduce mortality.
Case Reports
Case 1
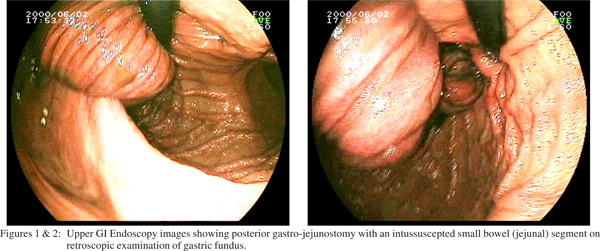
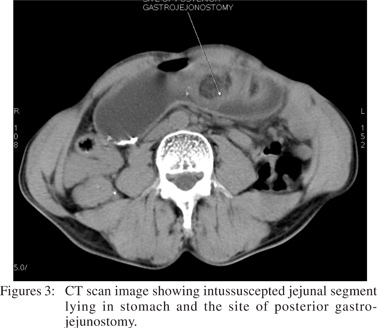
A 45 year old gentleman, presented to the emergency room with upper abdominal colicky pain, multiple episodes of vomiting and obstipation since 3 days. He had undergone a surgery (gastro-jejunostomy) for peptic ulcer disease 7 years ago. On examination, he was dehydrated and had upper abdominal midline scar of past gastro-jejunostomy. He had epigastric fullness, succussion splash and bowel sounds were absent. With a clinical diagnosis of gastric outlet obstruction on the background of post peptic ulcer surgery (gastrojejunostomy) status, he was evaluated further. Upper GI endoscopy was done, which revealed a dilated stomach with intussuscepted small bowel (jejunal segment) lying in the body of stomach (Figures 1 & 2). This finding was confirmed by ultrasonography and CT scan of the abdomen (Figures 3). Based on above findings, he was diagnosed to have acute retrograde JGI.
After initial correction of dehydration, dyselectrolytemia and gastric decompression (nasogatric aspiration), he was subjected to laparotomy. On abdominal exploration, he was found to have posterior gastro-jejunostomy through which efferent jejunal loop had intussuscepted into the stomach. The site of intussusception was approximately one and a half feet from GJ site. As the affected bowel was viable, the intussuscepted segment was manually reduced and efferent loop was fixed to afferent loop to prevent recurrence. Post operatively, patient had uncomplicated course and was started orally after 7 days of surgery. He was discharged on 9th postoperative day.
Case 2
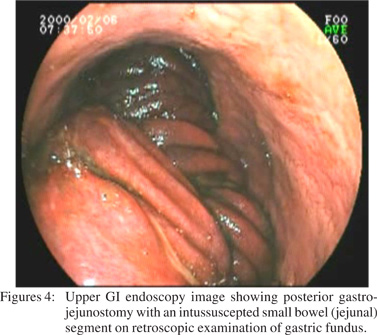
A 32 year old gentleman, presented with acute onset pain abdomen, vomiting for 10 days and haematemesis for 1 day. He had undergone surgery (gastro-jejunostomy) for peptic ulcer disease 5 years ago. On examination, he had an upper abdominal midline scar of past gastro-jejunostomy, epigastric fullness, palpable tender lump in the epigastrium and succussion splash. He was evaluated further by upper GI endoscopy, which revealed dilated stomach with intussuscepted small bowel (jejunal segment) lying in the body of stomach. Mucosa of intussuscepted segment was showing pre-gangrenous changes. (Figures 4).
He was subjected to emergency laparotomy and on abdominal exploration, he was found to have retro-colic gastrojejunostomy through which efferent jejunal loop had intussuscepted into the stomach. Though the mucosa of intussuscepted segment had pre-gangrenous changes, bowel wall was viable, and so the intussuscepted segment was manually reduced and efferent loop was fixed to afferent loop to prevent recurrence. Post operatively, patient had uncomplicated course and was discharged on 8th post-operative day.
Discussion
Retrograde JGI is a rare complication after gastric surgery and has been reported after every type of gastro-enteric anastomosis except Billroth I.[2] In 2004, Goverman and colleagues reported two cases of retrograde intussusceptions out of more than 600 Roux-en-Y gastric bypass procedures in their experience, which confirms the rarity of this disease.[5] Shackman proposed three anatomic types of JGI: type I involves the afferent loop (antegrade), type II the efferent loop (retrograde) and type III represents a combined form.[6] Type II or retrograde efferent loop intussusception is the most common (80%), with the two other types accounting for 10% each.[7] In the cases reported here, type II retrograde JGI was documented. This complication may occur at a variable period after original gastric surgery. The shortest interval reported is two days and the longest 30 years, with an average of 6 years.[8]
Patients with JGI can have acute fulminant or chronic recurrent presentation. The acute fulminant presentation is characterised by five classic manifestations: severe colicky epigastric pain, vomiting, hematemesis, a palpable abdominal mass and features of high intestinal obstruction. In the chronic recurrent type of presentation, patient experiences recurrent bouts of epigastric distress, nausea and colicky abdominal pain. The chronic recurrent variety is more common.[7] The causes of JGI are poorly understood. Various factors have been incriminated such as hyperacidity, long afferent loop, jejuna spasm with abnormal motility, increased intra-abdominal pressure and retrograde peristalsis.[2, 9] Other possible etiological factors include intestinal luminal prosthesis, suture or staple approximations or post-operative adhesions.10 In the cases presented, no intraluminal, intramural, or extraluminal cause could be detected. Retrograde peristalsis, which can occur in normal people prior to gastric surgery, seems to be accepted as the cause of type II JGI by most authors.[2, 9] Early diagnosis of the acute form is of paramount importance.[6] The clinical picture is almost diagnostic to the alert, sensitized physician. Plain Xray can be occasionally diagnostic, but endoscopy performed by someone familiar with this rare entity is certainly diagnostic.[11]
In the chronic form, the diagnosis is difficult. In these patients, the correct diagnosis may never get established. The main reason for this is that upper GI series or upper GI endoscopy must be performed during the symptomatic period for the diagnosis to be confirmed. The cases presented here, illustrate the use of gastroscopy in diagnosing this acute condition and planning timing of surgery by demonstrating bowel viability. The treatment of acute variety of JGI is prompt surgery. Delay in surgery beyond 48 hours is associated with an approximately 50% mortality. At operation if the intussuscepted jejunum is reducible and viable, then simple reduction should be performed. To prevent recurrence, the reduced jejunum should be fixed either to the afferent limb of gastro-jejunal anastomosis or to the transverse mesocolon. If the bowel is nonviable, it should be resected. The treatment of chronic recurrent variety of JGI is symptomatic. If symptoms persist then revision surgery is performed. Although recurrence after operative reduction is rare, it has been reported.[12]
In conclusion,retrograde jejunogastric intussusception is a well-recognised, but rare and potentially fatal, long-term complication of gastro-jejunostomy or Billroth – II reconstruction. Endoscopy performed by someone familiar with this rare entity is diagnostic. In case of acute fulminant presentation, early and prompt surgery can reduce mortality.
Reference
1. Varley CC, Dyer NH. Jejuno-gastric intussusceptions:gastroscopic diagnosis. Aust N Z J Med. 1977;7:515–7.
2. Archimandritis AJ, Hastzopoulas N, Hatzinikolaou N, Sougioultzis S, Kourtesas D, Papastrstis G, et al. Jejunogastric intussusception presented with hematemesis: a case presentation and review of literature. BMC Gastroenterol. 2001;1:1–4.
3. Jang WI, Kim ND, Bae SW. Intussusception into the enteroanastomosis after Billroth II gastric resection diagnosed by gastroscopy. J Korean Med Sci. 1989;4:51–4.
4. Kshirsagar AY, Shinde SL, Langade YB, Pujari SG, Jeur AS. Retrograde jejunogastric intussusception with strangulation after posterior gastrojejunostomy. MJAFI. 2008;64:282–3.
5. Goverman J, Greenwald M, Gellman L. Antiperistaltic (retrograde) intussusception after Roux-en-Y gastric bypass. Am J Surg. 2004;70:67–70.
6. Shackman R. Jejunogastric intussusception. Br J Surg. 1940;27:475–80.
7. Reyelt WP Jr, Anderson AA. Retrograde jejunogastric intussusception. Surg Gynecol Obstet. 1964;119:1305–11.
8. Wolukau-Wanambwa PP. An uncommon cause of haematemesisretrograde jejunogastric intussusception. Brit J Clin Prac. 1979;33:53–4.
9. Waits JO, Bearts RW Jr., Charboneau JW. Jejunogastric intussusception. Arch Surg. 1980;115:1449–52.
10. Ozdogan M, Hamaloglu E, Ozdemir A. Antegrade jejunojejunal intussusception after Roux-en-Y esophagojejunostomy as an unusual cause of postoperative intestinal obstruction: report of a case. Surg Today. 2001;31:355–7.
11. Kallen R, Graffner H, Jonsson Per-Ebbe J. Jejunogastric intussusception through the enteroanastomosis after gastric resection. A case report. Acta Chir Scand. 1986;152:637–40.
12. Menezes LT, D’Cruz A. Retrograde jejunogastric intussusceptions following gastric surgery. J Indian Med Assoc. 1986;84:310–11.