Introduction
Chronic Hepatitis B virus (CHB) infection is a global public health problem. There are 296 million HBV carriers with 1.5 million new infections occurring every year across the world and with a annual mortality of 820,000 individuals.1 Approximately, 15-40% patients with CHB will develop life-threatening consequences such as cirrhosis of liver and hepatocellular Carcinoma (HCC).2 High levels of hepatitis b(HBV) DNA is a marker of accelerated disease activity and is an independent risk factor for development of HCC. Persistent viral replication in patients with CHB may lead to development of liver fibrosis. Interestingly, fibrosis is the most important predictor of prognosis in CHB related liver disease and has a significant role in deciding treatment initiation.3
There are various invasive and non invasive modalities used to assess the degree of fibrosis. Till now, liver biopsy is still considered as the gold standard modality for detection of liver fibrosis. However, the liver biopsy (LB) has its own limitations including high intra and interobserver variability, sampling variability, and LB is an invasive method, with associated possible morbidity and mortality.4 Many non-invasive alternatives such as transient elastography have been developed to evaluate liver fibrosis and to monitor the progression of fibrosis.5
Transient elastography is based on the principle of Hooke’s law. Measurement of liver stiffness is performed and measured in kilopascals.6 However, 2D shear wave elastography (SWE) is relatively recent tool in the era of USG based liver fibrosis assessment which uses the usual 2D US probe to obtain accurate results, even in the presence of ascites and obesity. However, there are no definitive criteria for confirming the reliability of measurements observed in 2D-SWE techniques.8 Though there are many reports describing the use of TE in patients with chronic hepatitis B, there are fewer publications on the use of 2D-SWE. Hence, this study was carried out to assess the relationship of HBV DNA titre with the degree of liver fibrosis assessed by SWE in patients with CHB.
Materials and Methods
Methods: All consecutive HBV patients more than 14 years of age with detectable HBV DNA levels presenting to Department of Hepatology, SCB Medical College, Cuttack between August 2021 to January 2023 were included. Those with hepatocellular carcinoma, autoimmune hepatitis, alcoholic liver disease, NASH, pregnancy, gross ascites and small rib spaces were excluded. Informed consent was taken from all the patients. The study was approved by Institutional ethics committee of SCB Medical College, Cuttack, Odisha (IEC no 898 dt-3.8.2021).
Demographic and Clinical Data: Demographic details, clinical findings, and investigations were obtained and incorporated in a structured format. Patients or their relatives were explained in detail both verbally and in written form about the aims and objectives of the study. All patients underwent 2D SWE to estimate the median liver stiffness.
HBV DNA Quantitative Assay: It was done by Trueprep® AUTO v2 Universal Cartridge based Sample Prep Device (Molbio's INDIA ). Truelab micro PCR System is a nucleic acid amplification platform that works on Real Time Polymerase Chain Reaction (PCR) technology that enables near patient diagnosis through disposable, disease specific micro PCR chips and a portable, automated Truelab Real Time micro PCR analyzer. Analysis of the data was used to determine the concentration of the respective DNA with 95% probability of detection. LoD (limit of detection) was determined to be 55.92 IU/ml for HBV in plasma.
Shear Wave Elastography: Median liver stiffness was measured using LOGIQ shear wave elastography (GE LOGIQ™ S8 XDclear;C1-6-D convex transducer 16MHz, GE Healthcare, Milwaukee, WI, USA) as per our hospital protocol. Patient were advised fasting for atleast 4h before measurement to limit the effect of portal vein flow.9 The test was performed by the hepatologist with experience of performing over 1000 procedures.
A region of interest (ROI) was placed over an area of the liver, at least 1 cm below the liver capsule, taking care not to include large vasculature or biliary structures. Patients were in positioned in supine or slightly left decubitus position with right arm overhead, imaging approach targeting right liver lobe (segments 7 or 8) of the liver.10 Serial measurements, at least ten, were taken through multiple scans. Liver stiffness measurement (LSM) value was shown automatically on the machine. The median was measured, and the IQR/median ratio cutoff of 30% was taken for valid measurements. Liver fibrosis staging was done based on LSM values.11 Those with LSM values between 6.48 to 6.60 kpa were F1, 6.6 to 8.07 were F2, 8.07 to 9.31 were F3 and LSM value more than 9.31 were designated F4.11
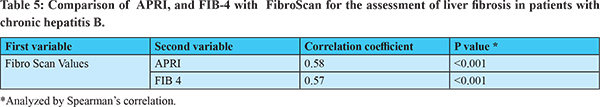
Aspartate platelet ratio index (APRI) and FIB4 index were calculated for all patients as per standard formulae.
Statistical Analysis: The quantitative data with continuous variables were expressed as mean ± standard deviation (S.D.) or median (interquartile range: IQR) as appropriate whereas categorical variables were expressed in terms of percentages. The significant difference of continuous variables were assessed by independent t test. Logistic regression analysis was done to find out significant independent predictors of fibrosis. Those variables which were found to be predictors of liver fibrosis on univariate analysis were taken into consideration for multivariate logistic regression analysis. All the statistical analysis were done by using SPSS version 20.0 (IBM, Chicago, USA).
Results
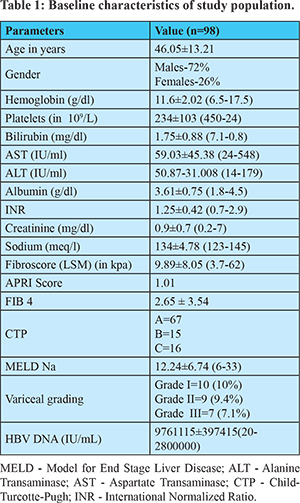
Baseline Clinical Characteristics: A total of 98 patients were evaluated in this cross sectional observational study.The baseline characteristics are depicted in Table 1. The mean age of patients was 46.05±13.21 years.The male to female ratiowas 2.76:1.The mean platelet counts, mean ALT, and mean serum albumin were 234±103×109/L, 50±87 IU/ml, 3.61±0.75 mg/dl respectively. Majority of patients were non-cirrhotics (n=67-68%) while 31(31%) were cirrhotics. Eighty seven (88.8%) patients had HBV DNA levels <106 IU/ml and 11 (11.2%) patients had DNA levels >106 IU/ml. The mean HBV DNA levels was 9761115±397415 IU/ml. Thirty seven (37.8%) patients had advanced fibrosis (=F3). The mean LSM was 9.89±8.05 kpa, mean APRI score was 1.01±1.32 and the mean FIB-4 was 2.65±3.54.
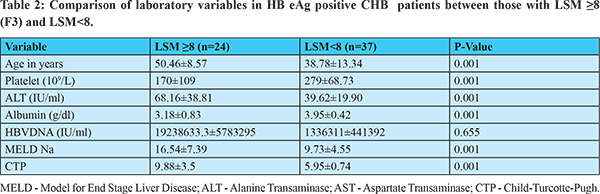
Comparison of Variables in HBeAg Positive CHB Patients Between Those with LSM =8 (=F3) and LSM<8: Table 2 reveals comparison of variables between HBeAg positive patients LSM =8(F3) versus those with LSM<8. Mean age was significantly higher among those with LSM =8 kpa as compared to those with LSM<8 kpa (50.46±8.57 vs 38.78±13.34; p<0.001). Similarly mean ALT (68.16 ± 38.81 vs 39.62 ± 19.90, p <001), mean MELD Na score (16.54 ± 7.39 vs 9.73±4.55, p<0.001) and mean CTP score (9.88±3.5 vs 5.95±0.74, p<0.001) were significantly higher among those with LSM=8 kpa compared to LSM<8 kpa where as mean serum albumin (3.18±0.83 vs 3.95±0.42, p<0.001) and mean platelet counts (170±109 vs 279±68.73, p<0.001) were significantly lower among those with LSM=8 kpa compared to those with LSM<8 kpa. Though HBV DNA was higher among those with LSM=8 kpa compared to LSM<8 kpa, the difference was not statistically significant.
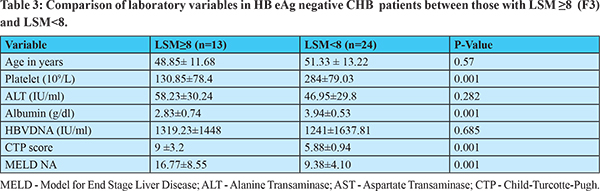
Comparison of Variables in HBeAg Negative CHB Patients Between Those with LSM =8 (=F3) and LSM<8: As depicted in Table 3, mean serum albumin (2.83±0.74 vs 3.94±0.53, p <0.001) and mean platelet count (130.85±78.4 vs 284±79.03, p<0.001) were significantly lower among those with LSM=8 kpa as compared to those with LSM<8 kpa, whereas mean CTP score (9±3.2 vs 5.88±0.94, p<0.001) and mean MELDNa score (16.77±8.55 vs 9.38±4.10, p<0.001) were significantly higher among those with LSM=8 kpa compared to LSM<8 kpa. Though HBV DNA was higher among those with LSM=8 kpa compared to LSM<8 kpa, the difference was statistically non-significant.
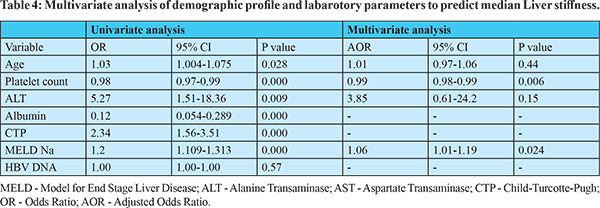
Predictor of Liver Fibrosis in Patients of Chronic Hepatitis B: As depicted in Table 4, age was a significant predictor of liver fibrosis (OR=1.039 with CI 1.004-1.075, p=0.028). Platelet count (OR=0.983, CI=0.976-0.990, p=0.001), and serum albumin (OR=0.125, CI=0.054-0.289, p=0.001) had significant inverse relationship with liver fibrosis. ALT levels (OR=5.278, CI=1.517-18.36, p=0.009), CTP score (OR=2.341, CI=1.560-3.511, p=0.000) and MELD Na score (OR=1.207, CI=1.109-1.313, p=0.000) were also significantly associated with liver fibrosis. HBV DNA (OR=1.000 with CI=1.000-1.000 p=0.602 ) and HBeAg (OR= 1.198, p=0.677) were not found to be significant predictors. However, on multi-variate analysis, platelet count (OR=0.999,CI=0.981-0.997, p=0.006) and MELD Na score (OR=1.064, CI=1.01-1.198, p=0.024) were the only parameters found to be significant independent predictors of liver fibrosis. As depicted in Table 5 both APRI (correlation coefficient 0.58, p <0.001) and FIB-4 (correlation coefficient 0.57, p <0.001) had excellent correlation with liver fibrosis.
Diagnostic Value of HBVDNA For Predicting Advanced Fibrosis (= F3): ROC curve analysis were done in all patients of CHB to determine the diagnostic accuracy of HBV DNA levels for predicting liver fibrosis,as shown Figure 1. The AUROC for HBV DNA to detect advanced fibrosis in patients with CHB was found to be 0.53 (95% CI 0.383-0.623; p=0.95). Hence, HBV DNA titre was not found to be reliable for predicting advanced fibrosis.
Diagnostic Value of APRI and FIB-4 Scores for Predicting Advanced Fibrosis (= F3): ROC curve analysis were done in all patients of CHB to determine the diagnostic accuracy of APRI and FIB-4 scores for predicting liver fibrosis, as shown Figure 2. The AUROC for APRI and FIB-4 scores to detect advanced fibrosis (LSM = 8) were 0.879 (95% CI 0.77-0.98; p=0.001) and 0.880 (95% CI 0.78-0.97; p=0.001) respectively. Hence APRI and FIB-4 scores were good predictors of advanced fibrosis.
Discussion
Liver fibrosis is key predictor of progression of liver disease in patients with chronic hepatitis B.12 Liver biopsy is still the gold standard method to assess degree of liver fibrosis but owing to its invasiveness, various non-invasive modalities like fibroscan and elastography have been developed and practised in the recent years.13 The utility of transient elastography in assessing the degree of fibrosis have been evaluated in earlier studies and liver stiffness values directly correlated with the degree of fibrosis.14 However, there were few studies assessing the correlation of Hepatitis B viral load with liver fibrosis.Hence, the current study was undertaken to as certain the relationship between HBV DNA and liver fibrosis using 2D SWE .
In our study, mean HBV DNA levels were higher in the group with chronic hepatitis B patients with LSM =8 kpa (F3) as compared to those with LSM <8 kpa but this was not statistically significant. HBV DNA was not found to be independent predictor of liver fibrosis in multivariate regression analysis. Although high replication of hepatitis B virus is an independent risk factor for development of cirrhosis and HCC (15), HBV DNA titre did not correlate with degree of fibrosis in our study. Various previous studies have made similar observations as ours. A study from Egypt by Saleh et.al observed that HBV DNA levels showed the highest levels in patients with advanced fibrosis as compared to earlier stages of fibrosis. However, it showed weak diagnostic performance in the differentiation between different stages of liver fibrosis and there was nonsignificant correlation between fibrosis score and viral load in their study.16 Another cross sectional study from Turkey also found poor diagnostic accuracy of HBV DNA >20000 IU/ml in detecting advanced fibrosis.17 However, an Iranian study with a very small cohort of 30 patients by Bizar et al found a significant correlation between HBV DNA and stage of liver fibrosis by histopathology.18 Another Iranian study of 236 treatment naive CHB patients showed that HBV DNA was correlated with liver fibrosis only in HBeAg negative CHB patients, but this correlation was not seen with HBeAg positive subjects.
In our study, mean age was significantly higher in patients with LSM =8 kpa as compared those with LSM<8, suggesting that age has a significant correlation with grade of fibrosis. This findings was also evident in many other studies.19,20,21 We also found that serum albumin was independent predictor of liver fibrosis and was significantly lower in patients with LSM=8 kpa as compared with LSM<8 kpa. Previous studies had also shown similar relationship of serum albumin with liver fibrosis.20,21,22 Hypoalbuminemia results from decreased synthesis of albumin from hepatocytes in patients of chronic liver disease, hence serum albumin levels correlated with degree of liver fibrosis.22,23
In the present study, platelet count was significantly lower patients with LSM=8 kpa (F3 fibrosis) as compared with LSM<8 kpa in both HBeAg positive and negative group. In addition, platelet count was a significant negative predictor of liver fibrosis. This association of low platelet count with liver fibrosis is also established in numerous previous studies.24,25,26 Reduced hepatocyte mass due to liver fibrosis resulting in decreased production of thrombopoietin might be the explanation for low platelet count in liver fibrosis. It was also found that APRI and FIB-4 were good predictors of advanced fibrosis. A recent study comprising of 253 patients also revealed that liver stiffness by 2DSWE was positively correlated with FIB-4 but not with APRI score.27
There are many strengths of current study. It comprises of real time data of CHB patients in relation to HBV DNA and liver fibrosis. Moreover, 2D SWE is relatively newer, more accurate modality of assessment of liver fibrosis and literature is limited. And also, such types of studies are scarce in this part of the world. However, this study has few limitations. Sample size was low. Results of study were not correlated with liver biopsy which is still the gold standard for assessment of liver fibrosis.
Conclusion
HBV DNA levels does not correlate with the degree of fibrosis in patients with chronic hepatitis B, in both HBeAg positive and HbeAg negative individuals. In addition HBV DNA is also not an independent predictor of fibrosis. Low platelelet count and hypoalbuminemiawere significant negative predictor of liver fibrosis. Large well designed future studies evaluating the predictive value of HBV DNA on liver fibrosis should be undertaken.
References
- States M, Strategic WHO, Group A, Grade T, Sage T. Weekly epidemiological record Relevé épidémiologique hebdomadaire. 2017;(27):369–92.
- Kew MC. Hepatitis B virus in the etiology of hepatocellular carcinoma. Perspective in Medical Virology. 2002;6:17–30.
- Wong GL. Prediction of fibrosis progression in chronic viral hepatitis. Clin Mol Hepatol. 2014 Sep;20(3):228-36.
- Puri P. Tackling the hepatitis B disease burdenin India. J Clin Exp Hepatol . 2014;4(4):312–9.
- Sugiyama M, Tanaka Y, Kurbanov F, Nakayama N, Mochida S, Mizokami M. Influences on hepatitis B virus replication by a naturally occurring mutation in the core gene. Virology. 2007;365(2):285–91.
- Arora A, Singh SP, Kumar A, Saraswat VA, Aggarwal R, Bangar M, et al. INASL Position Statements on Prevention, Diagnosis and Management of Hepatitis B Virus Infection in India: The Andaman Statements. J Clin Exp Hepatol. 2018;8(1):58–80.
- Sporea I, Sirli R, Deleanu A, Tudora A, Curescu M, Cornianu M, et al. Comparison of the liver stiffness measurement by transient elastography with the liver biopsy. World J Gastroenterol. 2008;14(42):6513–7.
- Guo HY, Liao M, Zheng J, Huang ZP, Xie SD. Two-dimensional shear wave elastography utilized in patients with ascites: a more reliable method than transient elastography for noninvasively detecting the liver stiffness-an original study with 170 patients. Ann Transl Med. 2023; 31;11(2):80.
- Barr, Richard G et al. “Update to the Society of Radiologists in Ultrasound Liver Elastography Consensus Statement. Radiology 2020;296(2): 263-274.
- Castera L. Non-invasive assessment of liver fibrosis in chronic hepatitis C. Hepatol Int. 2011;5(2):625–34.
- Sporea I, Bota S, Gradinaru-Tascau O, Sirli R, Popescu A, Jurchis A. Which are the cut-off values of 2D-Shear Wave Elastography (2D-SWE) liver stiffness measurements predicting different stages of liver fibrosis, considering Transient Elastography (TE) as the reference method. Eur J Radiol. 2014;83(3):5–6.
- Kim SU, Kim BK, Park JY, et al. Transient Elastography is Superior to FIB-4 in Assessing the Risk of Hepatocellular Carcinoma in Patients With Chronic Hepatitis B. Medicine (Baltimore) 2016;95:e3434.
- Fang JM, Cheng J, Chang MF, et al. Transient elastography versus liver biopsy: discordance in evaluations for fibrosis and steatosis from a pathology standpoint. Mod Pathol 2021;34:1955-62.
- Parikh P, Ryan JD, Tsochatzis EA. Fibrosis assessment in patients with chronic hepatitis B virus (HBV) infection. Ann Transl Med. 2017 Feb;5(3):40.
- Iloeje UH, Yang HI, Su J, Jen CL, You SL, Chen CJ. Predicting cirrhosis risk based on the level of circulating hepatitis B viral load. Gastroenterology. 2006;130(3):678–86.
- Saleh SA, Sayed M, Lotfy M, Abdellah HM, Hussein AM. Relation between hepatitis B viral load and liver fibrosis assessed using transient elastography in patients with chronic hepatitis B virus infection. Egypt Liver J. 2016;6(4):65–9.
- Danis N. Predictive value of FibroScan in detecting liver fibrosis in HBeAg negative patients with chronic hepatitis B whose HBV DNA 2000-20000 IU/ml with ALT 1-2 times the upper limit of normal and those with HBV DNA >20000 IU/ml and normal ALT. North Clin Istanbul. 2021;8(6):568-57.
- Biazar T, Yahyapour Y, Hasanjani MR, Roushan, Rajabnia R, Sadeghi M, et al. Relationship between hepatitis B DNA viral load in the liver and its histology in patients with chronic hepatitis B. Casp J Intern Med. 2015;6(4):209–12.
- Wang CC, Lim LY, Deubner H, Tapia K, Lau AWY, Manansala J, et al. Factors predictive of significant hepatic fibrosis in adults with chronic hepatitis B and normal serum ALT. J Clin Gastroenterol. 2008;42(7):820–6.
- Mohamadnejad M, Montazeri G, Fazlollahi A, Zamani F, Nasiri J, Nobakht H, et al. Noninvasive markers of liver fibrosis and inflammation in chronic hepatitis B-virus related liver disease. Am J Gastroenterol. 2006;101(11):2537–45.
- Demir NA, Kolgelier S, Ozcimen S, Gungor G, Sumer S, Demir LS, et al. Evaluation of the relation between hepatic fibrosis and basic laboratory parameters in patients with chronic hepatitis B fibrosis and basic laboratory parameters. Hepat Mon. 2014;14(4):1–5.
- Maulidia VNR, Wardhani P, Setyoboedi B. AST, ALT and Albumin Level in Chronic Hepatitis B Patients with and without Complications of Cirrhosis and Hepatocellular Carcinoma. Indones J Clin Pathol Med Lab. 2020;26(3):344–9.
- Henricksen JH, Siemssen O, Krintel JJ, Malchow-Møller A, Bendtsen F, Ring-Larsen H. Dynamics of albumin in plasma and ascites fluid in patients with cirrhosis. Journal of Hepatology, 2001; 16: 53-60.
- Nwokediuko S. Quantitative Platelet Abnormalities in Patients With Hepatitis B Virus-Related Liver Disease. Gastroenterol Res. 2009;1–10.
- Joo EJ, Chang Y, Yeom JS, Lee YG, Ryu S. Hepatitis B infection is associated with an increased incidence of thrombocytopenia in healthy adults without cirrhosis. J Viral Hepat. 2017;24(3):253–8.
- Karasu Z, Tekin F, Ersoz G, Gunsar F, Batur Y, Ilter T, Akarca US. Liver fibrosis is associated with decreased peripheral platelet count in patients with chronic hepatitis B and C. Dig Dis Sci. 2007;52(6):1535-9.
- Kavak, S., Kaya, S., Senol, A. et al. Evaluation of liver fibrosis in chronic hepatitis B patients with 2D shear wave elastography with propagation map guidance: a single-centre study. BMC Med Imaging 2022; 18;22(1):50.