48uep6bbphidvals|426
48uep6bbph|2000F98CTab_Articles|Fulltext
Introduction
Fetus-in-fetu (FIF) is a rare congenital condition of undecided etiology where a malformed fetus like structure is found inside the body of its twin. Owing to its rarity, FIF is not usually considered as a possibility in an infant presenting with an abdominal mass. This case of FIF is reported for its unusual presentation exhibiting a sudden spurt in size, which has not been reported in literature so far and the difficulty to differentiate it from a malignant teratoma.
Case Report
A four and a half month old girl weighing 4.5 kilograms, presented with an enlarging lump in abdomen since two and half months. The lump was first noticed in the right upper abdomen which gradually enlarged over two months, and then rapidly increased in size over the next 10-15 days to cover almost the entire abdomen accompanied with significant loss of appetite. There was no fever, urinary or bowel complaints. The mother of the child did not give history of multiple pregnancies.
General physical examination, respiratory and cardiovascular systems were normal. Abdominal examination revealed a well defined, 15×15 cm firm, irregular, fixed, non tender lump in the right side of abdomen crossing the midline. Routine hematological investigations were unremarkable.
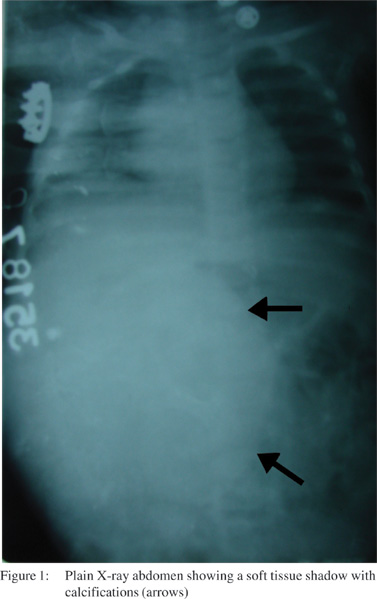
Plain X-ray of the abdomen showed a soft tissue shadow with calcifications in right half of abdomen (Figure 1). Ultrasonography confirmed a large, well encapsulated, echogenic mass inferior to the liver and anterior to the right kidney with areas of calcification surrounded by a hypoechoic ring. Liver, kidneys, spleen and uterus were normal. FNAC from the mass was suggestive of teratoma or neuroblastoma. The patient was planned for a CECT scan of the abdomen, but due to sudden spurt in size of the mass causing respiratory discomfort, malignant teratoma was suspected and a plan for immediate abdominal exploration was made, anticipating inoperability if the surgery was delayed.
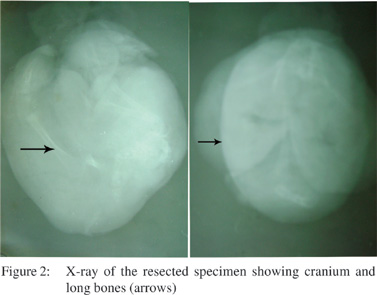
Laparotomy revealed a retroperitoneal lump within a sac containing small amount of green coloured thick fluid. The sac was densely adherent to the posterior surface of pancreas and duodenum, but could be dissected free. It was removed completely after separating it from the adherent right kidney and renal vessels, inferior vena cava (IVC) and the liver hilum. The pedicle of the lump was seen to converge on to the IVC, although no distinct vascular communication was appreciated. The uterus and adnexae of the child were normal. The postoperative course was uneventful and the child was discharged on the eighth post-operative day. The specimen had three vestigial arm like structures. Radiograph of the specimen showed cranium and long bones but no vertebral column. (Figure 2).
The lump was a maldeveloped fetus measuring 18×10×9 cm with three bosselations and three rudimentary limbs, weighing 480 grams. Histopathological examination revealed a partially developed (non osseous) vertebral column confirming the diagnosis of FIF.
Discussion
FIF is a mystery in medical science with scarce reports in literature. It is a rare congenital condition occurring commonly in families with multiple births.[1] FIF was reported first by Meckel in 1800, and although recently published reports quote the number of reported cases to be less than 100 worldwide[2,3,4] we could retrieve nearly 160 cases from published English literature of which 22 cases have been reported from India . It is debatable whether it is a distinct entity or a highly differentiated variant of teratoma.[3,5,6,7] There are two theories regarding development of FIF. The first theory states that FIF results from a modified process of twining. The other is the Willis theory of inclusion of monozygotic diamniotic twin within the bearer. Of these two theories, the latter is widely accepted.[8]
Although FIF has usually been identified in infancy, it has been reported in children as well as in adults.[9,10] Mostly the mass is located in the retroperitoneum[3,4,9,11] as in our case, due to its close relation with the vitelline circulation. However, FIF has been reported to occur at other locations[1,3,9,11] such as within the cranium, oral cavity, neck, mediastinum, lung, liver,[12] pelvis and scrotum. Usually only one fetus is present, but multiple FIF have also been reported.[7,13] It is commonly enclosed in fluid filled capsule without major vascular connections,[3,13,14]
as was in the case presented. FIF does not have neoplastic potential.
Difficulty lies in differentiating FIF from retroperitoneal teratomas, to which it may resemble closely, clinically and radiologically. Retroperitoneal teratomas are rare and effect children in first decade of their life. Teratomas are twice as common in females as in males. Most of retroperitoneal teratomas are benign and progress slowly but with malignantchange they tend to progress rapidly.[15] Rapid progression is not a feature of FIF and to the best of our knowledge this is the first ever reported case of FIF which presented with rapid progression in size, raising suspicion of malignant teratoma.
Moreover, non visualization of vertebral column on X-ray further decreased the suspicion of the possibility of FIF. FIF is differentiated from teratoma by the presence of an axial skeleton and organoid formations within the mass;1 however, maturation of all organs may not be parallel, with some being incompletely developed. Although X-ray and USG are helpful in diagnosing FIF,7 the diagnostic yield is greatly increased by CT and MRI. It is even possible to diagnose it prenatally. The treatment of FIF is by resection, as was done in the present case.
References
- De Lagausie P, De Napoli Cocci S, Stempfle N, Truong QD, Vuillard E, Ferkadji L, et al. Highly differentiated teratoma and fetus-in-fetu: a single pathology? J Pediatr Surg. 1997;32:115–6.
- Kahloul N, Adouani M, Khattat N, Allani H, Krichen I, Zakhama A, et al. Fetus in fetu: a case report. Arch Pediatr. 2010;17:249–52.
- Khalifa NM, Maximous DW, Abd-Elsayed AA. Fetus in fetu: a case report. J Med Case Reports. 2008;2:2.
- Kim JW, Park SH, Park SS, Wang KC, Cho BK, Kim SY et al. Fetus-in-fetu in the cranium of a 4-month-old boy: histopathology and short tandem repeat polymorphism-based genotyping. Case report. J Neurosurg Pediatr. 2008;1:410–4.
- Arlikar JD, Mane SB, Dhende NP, Sanghavi Y, Valand AG, Butale PR. Fetus in fetu: two case reports and review of literature. Pediatr Surg Int. 2009;25:289–92.
- Marnet D, Vinchon M, Kerdraon O, Joriot S, Chafiotte C, Dhellemmes P. Antenatal diagnosis of a third ventricular mass: fetus in fetu or teratoma? Childs Nerv Syst. 2008;24:887–91.
- Balogun BO, Bankole MA, Akinola RA, Akintomide TE, Olayiwola B, Jinadu FO. Fetus-in-fetu. Afr J Paediatr Surg. 2008;5:93–5.
- Eng HL, Chuang JH, Lee TY, Chen WJ. Fetus in fetu: a case report and review of the literature. J Pediatr Surg. 1989;24:296–9.
- Abdur-Rahman LO, Abdul-Kadir AY, Rahman AG. Fetus-in-fetu in a 6-month-old. Afr J Paediatr Surg. 2008;5:96–8.10. Mohan H, Chhabra S, Handa U. Fetus-in-fetu: a rare entity. Fetal Diagn Ther. 2007;22:195–7.
- Karaman I, Erdoðan D, Ozalevli S, Karaman A, Cavuþoðlu YH, Aslan MK, et al. Fetus in fetu: A report of two cases. J Indian Assoc Pediatr Surg. 2008;13:30–2.
- Magnus KG, Millar AJ, Sinclair-Smith CC, Rode H. Intrahepatic fetus-in-fetu: a case report and review of the literature. J Pediatr Surg. 1999;34:1861–4.
- Kajbafzadeh AM, Baharnoori M. Fetus in fetu. Can J Urol. 2006;13:3277–8.
- Daga BV, Chaudhary VA, Ingle AS, Dhamangaokar VB, Jadhav DP, Kulkarni PA. Double fetus-in-fetu: CT scan diagnosis in an adult. Indian J Radiol Imaging. 2009;19:216–8.
- Taori K, Rathod J, Deshmukh A, Sheorain VS, Jawale R, Sanyal
R et al. Primary extragonadal retroperitoneal teratoma in an adult. Br J Radiol. 2006;79:e120–2.