48uep6bbphidvals|436
48uep6bbph|2000F98CTab_Articles|Fulltext
Proton pump inhibitors (PPIs) are substituted benzimidazole
derivatives and are the most potent suppressors of gastric
acid. Pantoprazole is the prototype proton pump inhibitor which
was approved for patient prescription in the late 1980s. Since
then PPIs became one of the most widely prescribed classes of
medications. Several studies have reported overusage of PPIs
in hospital as well as at the time of discharge after
hospitalization with most of the indications being
inappropriate.[1,2,3, 4,5]
Reports published in the initial decade of the clinical usage
of PPIs, have shown that the risk of adverse effects from these drugs is low and most of the adverse events are minor and selflimiting.[6,7,8,910] The relatively good safety profile of this class of
drugs could be one of the reasons for the over prescription of
these drugs. But polypharmacy in this way can lead to potential
undesirable drug-drug interactions and also results in an
increase of the health care costs.
Recently several reports have highlighted certain clinically
relevant adverse events of a serious note in relation to PPI
usage (listed in Table 1). In light of these findings, it is imperative
to analyze the data regarding the adverse effects and safety
profile of PPIs which will help us in understanding the
magnitude of the problem and also rationalize our approach
while prescribing medications to the patients.
Table 1: Adverse events of clinical significance reported with
PPIs

Effect of PPI – Clopidogrel interaction on
thrombotic events
Clopidogrel, a thienopyridine derivative, is a prodrug which is
metabolized by hepatic cytochrome P4502C19 to its active
metabolite which inhibits platelet aggregation by selectively
and irreversibly binding to the purinergic P2Y12 receptors on
the platelet surface. PPIs are also metabolized in the liver from
an active to inactive state by the same CYP2C19 isoenzyme.
Thus PPIs and clopidogrel compete for the same subset of cyt
P-450 isoenzymes (depicted in Figure 1).
Gilard et al[11] first reported reduced effectiveness of
clopidogrel in patients receiving PPIs by assessing the
vasodilator stimulated phosphoprotein (VASP)
phosphorylation index. They found significantly higher VASP
values in PPI users compared to non-users, higher values
indicating a diminished biological action of clopidogrel on
platelet function. Subsequently the same research group
conducted the OCLA study which was a prospective, doubleblind,
placebo-controlled, randomized trial in which they
demonstrated a signiûcantly decreased clopidogrel inhibitory
effect on platelet P2Y12 as assessed by VASP phosphorylation
test in patients receiving omeprazole 20 mg/day for 7 days
compared to placebo.[12]

Though all PPIs are metabolized by CYP2C19, the
clopidogrel-PPI interaction was not uniform among the
different PPIs. Only omeprazole but not pantoprazole or
esomeprazole was found to have attenuating effect on the
platelet response to clopidogrel in a cross-sectional
observational study in which multiple electrode platelet
aggregometry (MEA) was used to measure adenosine
diphosphate (ADP)-induced platelet aggregation.[13] The
influence of omeprazole and pantoprazole on a high 150-mg
clopidogrel maintenance dose was assessed in the PACA study
which is a prospective, randomized controlled trial and it was
found that patients receiving pantoprazole had a significantly
better platelet response to clopidogrel as compared to those
receiving omeprazole, as assessed by the platelet reactivity
index vasoactive stimulated phosphoprotein (PRI VASP).[14] In
another study where in vitro platelet aggregation was
measured, it was found that omeprazole and rabeprazole but
not lansoprazole significantly attenuated the anti-platelet
function of clopidogrel in rapid metabolizers of CYP2C19
whereas in decreased metabolizers there was no significant
change with any of these of three PPIs used concomitantly
with clopidogrel.[15]
Following these mechanistic in vitro studies which have
demonstrated conclusively the PPI-clopidogrel interaction,
studies were carried out to estimate the relevance and
magnitude of this interaction with regards to clinical outcomes.
A systematic review of all studies reporting clinical outcomes
has been performed and this included 18 studies investigating
the PPI-clopidogrel interaction.[16] 13 of these studies were
judged to be of a low a quality and 5 studies to be of a moderate
or high quality. Out these 18 studies, 10 studies reported an
increased risk of thrombotic events/ adverse cardiovascular
outcomes with concomitant use of PPIs and clopidogrel. However all these 10 studies were judged to be of a low quality.
The 5 studies which were judged to be of a moderate or high
quality reported no statistically significant association of PPIclopidogrel
interaction leading to an adverse clinical outcome.
In a meta-analysis which evaluated the effect of PPIs on
the clinical outcomes in patients treated with clopidogrel, 159138
patients from 25 studies were included.[17] It was found that the
concomitant use of PPIs with clopidogrel resulted in an increase
in adverse cardiovascular events but it did not influence the
risk of mortality. However there was significant heterogeneity
among the studies included indicating that the evidence was biased, confounded or inconsistent.
Data from the COGENT trial is the best quality evidence
that is available regarding the clinical outcomes of PPIclopidogrel
interaction.[18] In the COGENT trial 5000 patients
with an indication for a dual antiplatelet therapy following acute
coronary syndrome or stent implantation were planned to be
randomly assigned to omeprazole or placebo. The dual primary
end points were gastrointestinal (a composite of overt or occult
bleeding, symptomatic gastroduodenal ulcers or erosions,
obstruction or perforation) and cardiovascular (a composite of
death from cardiovascular causes, nonfatal myocardial
infarction, revascularization or stroke). The trial was terminated
prematurely owing to loss of finances by the study sponsor
and only 3873 patients were included. Patients in the omeprazole
group had significantly lesser primary GI end points compared
to placebo whereas the number of patients reaching the primary
cardiovascular end point was similar in both the groups. The
authors concluded that among patients receiving aspirin plus
clopidogrel, the prophylactic use of a PPI reduced the rate of
upper gastrointestinal bleeding, and though there was no
apparent cardiovascular interaction between clopidogrel and
omeprazole, the results did not rule out a clinically meaningful
difference in cardiovascular events due to use of a PPI.
To conclude, there is surrogate laboratory data supporting
the biologically plausible PPI-clopidogrel interaction, however
the available clinical evidence for the same is questionable
with the high quality trials not showing detrimental clinical
effects.
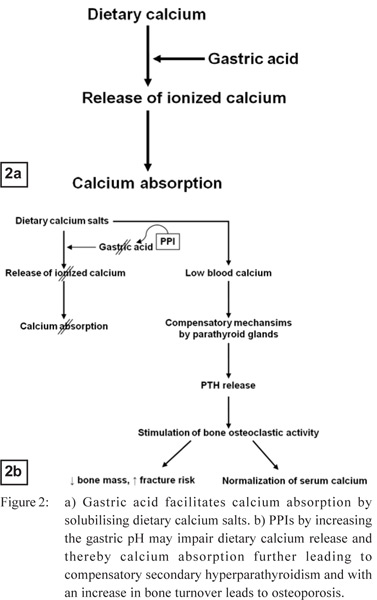
PPIs and bone health
Calcium absorption requires an acidic mileu in the stomach
and upper small bowel to solubilise dietary calcium salts and
facilitate the release of ionized calcium from insoluble calcium
salts.[19,20] Physiologic compensatory mechanisms occur in
response to impaired calcium absorption leading to secondary
hyperparathyroidism which further can lead to increase in
osteoclastic bone resorption, increase in skeletal turnover,
decrease in bone mass and thence may result in an increase of
risk of fractures (depicted in Figure 2).
There is a paucity of long-term studies with regards to the
effects of PPIs on calcium absorption. Short-term studies
revealed a highly variable effect of gastric acid suppression on
calcium absorption and bone turnover.[21,22,23,24] At the level of
osteoclasts, omeprazole at high concentrations was found to
interact with the vacuolar adenosine triphosphatases on
osteoclasts in vitro and in rodents, which has an
antiresorptive effect on bones.[25] However, long-term
administration to rats resulted in lower bone density.
Following the initial large population health database
derived case-control studies published by Yang et al[26] and
Vestergaard et al[27] in 2006, various other case-control studies
as well as cohort studies have been done investigating the
relationship between PPI usage and the risk of developing
osteoporosis and bone fractures. No randomized controlled
trial has been performed investigating the same. Two metaanalyses
have been published recently regarding the risk of
fractures with acid suppressive medications.[28,29]
Kwok et al found a significantly increased risk for spine
fractures (odds ratio [OR] 1.50, 95% confidence interval [CI]
1.32–1.72), hip fractures (OR 1.23, 95% CI 1.11–1.36) and
fractures overall (OR 1.20 95% CI 1.11–1.30) with usage of PPIs.
Except for the data regarding spine fractures, substantial
heterogeneity was found in the rest of the analyses in this
study.[28] Yu et al found an increased risk of hip fractures (relative
risk [RR] 1.30, 95% CI, 1.19-1.43),spine fractures (RR 1.56, 95%
CI, 1.31-1.85) and any-site fractures (RR 1.16, 95% CI, 1.04-
1.30) among PPI users.[29] They reported similar findings in men
and women as well as with duration of PPI usage of less than
or more than 1 year. The authors also acknowledged a possibility
of residual confounding bias in this analysis.
Thus, with the current available evidence there appears to
be an increased risk of fractures with PPI usage, the risk being
modest at best. However, with concerns regarding the trials’
methodology, properly designed prospective studies are
needed to exactly quantify the risk of bone disease with PPI
usage.
PPIs and pneumonia
Gastric acid kills ingested bacteria and thus prevents bacterial
colonization (other than Helicobacter pylori) of upper
gastrointestinal tract. Gastric bacterial overgrowth has been
documented in situations of profound acid suppression.[30,31,32] This may further lead to development of respiratory colonization
and pneumonia following microaspiration during episodes of
gastroesophageal reflux especially in patients with
compromised oropharyngeal protective reflexes.
Laheij et al have performed a population based cohort study
to examine the association between the use of gastric acid–
suppressive drugs and community-acquired pneumonia and it
is the first large scale study of such kind.[33] They found that
the incidence of pneumonia was about 4.5 times higher in
patients who received acid-suppressive drugs (both PPIs
and histamine-2-receptor antagonists [H2RA]) compared to
those who did not receive them. Subsequently several other
observational studies investigating the association between
PPIs and risk of community-acquired pneumonia have been
reported.
A meta-analysis has been performed recently examining
the association between risk of community-acquired
pneumonia and PPI use in adults.[34] They found a modest
increase in the risk of community-acquired pneumonia with
PPI use (OR 1.36, 95% CI 1.12–1.65). However there was
significant heterogeneity among the studies included which
hindered the investigators in arriving at definitive conclusions.
In an exploratory subgroup analysis, shorter duration of PPI
use was associated with an increased odds of communityacquired
pneumonia [OR 1.92, 95% CI 1.40–2.63] compared to
chronic usage [OR 1.11, 95% CI 0.90–1.38]. This is against the
proposed theory of strong acid suppression leading to gastric
bacterial colonization as the first step in the pathogenesis of
pneumonia.
Hospital-acquired pneumonia has also been reported to
occur at a higher incidence in patients exposed to acidsuppressive
drugs than in the unexposed group (4.6% vs 2.0%)
with the adjusted odds ratio for pneumonia being 1.3 (95% CI
1.1–1.4) in the exposed group.[35] This association was significant
for PPIs but not H2RAs. However this study was conducted in
non-ventilated patients. There is paucity of data in this regard
in ventilated patients especially with the currently available
potent intravenous PPIs.
To summarize, though biologically plausible, the overall
evidence is suggestive of a modest increase in the risk of pneumonia with use of PPIs. However definite conclusions
cannot be made because of the quality of evidence available.
PPIs and enteric infections
Clostridium difficile is a gram-positive, anaerobic sporeforming
bacillus and is one of the most common causes of
nosocomial diarrhoea and also has an increasing presence as a
cause of community-acquired pathogen. Traditional risk factors
for C.difficile associated diarrhoea (CDAD) are exposure to
antibiotics, increased underlying disease severity, old age,
immunodeficiency states and prolonged hospital stay.[36,37]
There are several recent studies which have examined the
relationship between PPI usage and CDAD. A positive
association between PPI usage and nosocomial[38,39,40,41] or
community-associated[42,43] CDAD has been reported in some
studies, but there have been some studies which reported no
such association.[44,45,46,47] In a recent meta-analysis which included
12 studies evaluating 2,948 patients with C.difficile, a
significant relationship between PPI use and C diffcile infection
was found, with a pooled odds ratio of 1.96 (95% CI 1.28–
3.00).[48] However there was significant heterogeneity between
the studies included. Though the data analyzed showed an
association between PPI usage and CDAD, it was insufficient
to establish causality.
Howell et al conducted a pharmaco epidemiologic cohort
study investigating the relationship between gastric acid
suppression and the risk of nosocomial CDAD.[49] They found
a significant dose-response with more aggressive acidsuppression
associated with higher odds ratios of developing
CDAD. This evidence of a dose-response effect provided
support for the potentially causal nature of iatrogenic acid
suppression in the development of nosocomial CDAD.
In addition to CDAD, an association between other enteric
infections and PPI usage has also been observed. This
relationship has been evaluated in a recent meta-analysis of
11,280 patients from 6 studies.[48] The diagnosis of enteric
infection was established either by microbial isolation of the
pathogen (Salmonella, Campylobacter, Escherichia coli, C
difficile, Shigella) or a clinical definition based on acute selflimited
diarrheal disease. All 6 studies associated an increased
risk of acute bacterial enteric infection with use of PPIs (pooled
OR 3.33, 95% CI 1.84–6.02), but there was significant
heterogeneity among the studies included. Though an association between enteric infections and PPI usage has been
demonstrated, the available evidence is insufficient to establish
causality.
The mechanism by which PPIs promote C. difficile infection
is not clear. Though it has been widely postulated that acidic
pH of the gastric contents may kill C. difficile spores and PPIs
nullify this effect, recently evidence has been generated against
this hypothesis. Nerandzic et al demonstrated survival of C.
difficile spores in nonbilious gastric contents with acidic pH.[50] This raises the question whether the association found in some studies between CDAD and PPI usage is due to some
unidentified confounders or whether the mechanism of
interaction between PPI and CDAD is true but unknown yet.
PPIs and pregnancy
Omeprazole is listed under class B risk category whereas other
PPIs are listed under class C risk category for usage in
pregnancy. In a recent meta-analysis 7 observational studies
were included and data from 134,940 patients of whom 1,530
were exposed and 133,410 not exposed to PPIs, was analyzed.[51] No association was found between PPIs and major congenital
birth defects (OR 1.12, 95% CI 0.86-1.45), spontaneous abortions (OR=1.29, 95% CI: 0.84-1.97), or preterm delivery
(OR=1.13, 95% CI: 0.96-1.33). Secondary analysis with
omeprazole alone also revealed no association with any major
congenital malformations (OR 1.17, 95% CI 0.90-1.53).
In a subsequently published study, Pasternak and Hviid
assessed the association between exposure to PPIs during
pregnancy and the risk of major birth defects evident in a large
cohort of live births over a 13 year period.[52] They found no
significant association between exposure to PPIs in the first
trimester of pregnancy and any major birth defects (OR 1.10,
95% CI 0.91 to 1.34). Similar results were found in secondary
analyses of exposure to different individual PPIs. They also
found that women who had received PPIs within 4 weeks before
conception but not enough doses to have a theoretical chance
of continued exposure beyond conception, were at increased
risk of having infants with major birth defects (adjusted
prevalence OR 1.53; 95% CI, 1.22 to 1.92). However, among
women who received enough doses within 4 weeks before
conception to have a theoretical chance of exposure in the first
trimester, the exposure to PPIs was not significantly associated
with major birth defects (adjusted prevalence OR 1.12; 95% CI,
0.94 to 1.35). The authors opined that the incongruent results
regarding the risk of birth defects in women who were exposed
to PPIs within 4 weeks before conception could either be
unmeasured confounding or may just be by chance.
PPIs and acute interstitial nephritis (AIN)
Several reports have implicated PPIs in causing AIN. The exact
pathogenesis of PPI-induced AIN is not yet known though it
is thought to be triggered by a hypersensitivity mmune
reaction to the drug or one of its metabolites. Usually patients
present with non-specific symptoms like fatigue, nausea,
malaise, weight loss and urinary examination usually reveals
pyuria, eosinophiluria or proteinuria. Sierra et al performed a
systematic review regarding PPI associated AIN and they found
64 reported cases of PPI related AIN, 59 of which were biopsy
proven.[53] All of the PPIs, except for dexalansoprazole (which
was not available at that time), were implicated, suggesting a
class effect. They found that the available evidence may
suggest a low-prevalence association , however it is insufficient
to establish a causal relationship.
PPIs and B12 deficiency
Gastric acidity is important for the absorption of vitamin B12.
Gastric acid along with pepsin facilitates the release of the
dietary vitamin B12 which is tightly bound to protein.[54] PPIs
may interfere with this process by increasing the gastric pH.
Accordingly PPIs have been demonstrated to decrease
absorption of protein-bound vitamin B12 in the majority of
studies,[55,56,57] however there are a few studies which differed.[58] Investigations regarding the association between long-term
PPI use and vitamin B12 deficiency revealed more inconsistent
results.[57,59,60,61]
Valuck and Ruscin performed a case-control study to
investigate the association between gastric acid suppression
and B12 deficiency in older adults aged 65 years or more.[59] They found that chronic current but not past or current shortterm
use of H2RA/PPI was associated with a significantly
increased risk of vitamin B12 deficiency (OR 4.45; 95% CI 1.47-
13.34). Termanini et al have performed a prospective cohort
study of 131 patients who received long-term PPI/ H2RA
therapy for Zollinger–Ellison syndrome, and found a significant
decrease of serum vitamin B12 levels in patients who were on
omeprazole with the mean duration of treatment being 4.5
years.[60] The decrease occurred primarily among those with
omeprazole-induced, sustained hyposecretion or complete
achlorhydria, indicating that it was a specific effect of acid
suppression. However in another long term prospective study
by den Elzen et al in 125 patients aged 65 yr and above who
received PPIs for more than 3 yr, no differences in mean vitamin
B12 levels were observed between the long-term proton pump
inhibitor users and their partners.[61] Schenk et al evaluated the
absorption of protein-bound and unbound cyanocobalamin
before and during treatment with omeprazole, and cobalamin
levels in patients on long-term treatment with omeprazole, the
mean treatment duration being 56 months.[57] Though they found
a decrease in the protein-bound vitamin B12 absorption among
subjects on short-term PPI therapy, there were no significant
differences in mean serum levels of vitamin B12 levels with
long-term omeprazole therapy.
PPIs and hypomagnesaemia
Magnesium is a predominantly intracellular cation which has
an important role in various biological processes like membrane
stabilization, neuromuscular excitability, oxidative
phosporylation and nucleic acid synthesis. It is absorbed in
the intestine mainly by passive diffusion through the
paracellular route, an alternative active transport mechanism
has also been identified recently.[62] Renal handling of
magnesium plays an important role in regulating body
magnesium status.
Recently several reports have thrown light of an association
of hypomagnesaemia with PPI use, irrespective of the type of
drug used indicating a class effect.[63,64] Prompt resolution of
the hypomagnesaemia usually occurred within days of
stopping the incriminated PPIs and also recurrence of
hypomagnesaemia was demonstrated with rechallenge of PPIs.
The true prevalence of PPI related hypomagnesaemia or the
risk of inducing hypomagnesaemia with PPI usage is not known
as it was never studied in a systematic fashion. Patients usually
have non-specific symptoms such as anorexia, nausea, tremor,
apathy, depression, agitation, confusion with milder cases of
hypomagnesaemia being usually asymptomatic. One should
be alert to investigate for hypomagnesaemia in conditions of
difficult to correct hypokalaemia and hypocalcaemia.
The exact mechanism of hypomagnesaemia in patients with
PPI usage is not known. Renal magnesium handling was found
to be normal with PPI usage. No apparent difference was found
in short term studies of intestinal absorption of magnesium
with PPI usage.[65,66] However, there is no data to make
conclusions regarding magnesium absorption with long term
usage of PPIs as well as regarding fecal losses of magnesium
with usage of PPIs.
PPIs and iron absorption
Dietary iron is present in food either as haem iron or non-haem
iron, with the latter supplying about 2/3rds of the dietary iron
requirements. Majority of the non-haem iron is in the ferric
form and gastric hydrochloric acid plays an important role in
its optimum absorption by reducing ferric iron to the more
soluble ferrous form. In an in vitro study investigating the
capacity of gastric juice produced by pentagastrin challenge
to release radioiron through solubilisation from biosynthetically
labelled bread, it was shown that below pH 2.5 there was a
linear relation between pH and percentage solubility of dietary
non-haem iron.[67] Similarly close correlation between iron
absorption and the capacity of gastric juice to release dietary
iron was demonstrated in an in vivo study.[67] However, longterm
use of PPIs has not been reported to compromise iron
status in normal subjects[68] as well as in patients with Zollinger-
Ellison syndrome.[69] In another study done in fully treated
patients of hereditary hemochromatosis, it was found that shortterm
administration of PPIs resulted in a significant reduction
in the absorption of non-haem iron and also led to a significant
reduction in annual phlebotomy requirements in patients on
long-term PPIs.[70]
PPIs and risk of neoplasia
PPI therapy leads to parietal cell inhibition and acid
suppression. The physiological negative feedback effect of
acidic pH on gastric secretion is thus lost leading to
hypergastrinemia. Gastrin has been found to have trophic effect
on epithelial cell growth and proliferation in stomach, colon
and pancreas.[71,72,73,74,75,76,77,78] These are mainly animal studies and studies
in tumour cell lines. However no human clinical studies have
clearly established an increased risk of cancer at any of these
sites due to hypergastrinemia occurring due to PPI use.
Hyperplasia of enterochromaffin-like cells latter on leading
to carcinoid formation has been reported in rats in response to
hypergastrinemia occurring in relation to profound acid
suppression.[79] However, carcinoid formation in the setting of
PPI use has not been reported in humans and only diffuse,
linear, or micronodular hyperplasia of enterochromaffin-like cells
was observed in 10–30% of chronic PPI users, particularly in H
pylori positive patients with moderate to severe inflammation
of body mucosa often with atrophic changes and more markedly
increased gastrin levels.[80] Sporadic fundic gland polyps (FGPs)
have been reported to occur with long term PPI maintenance
therapy. FGPs occur due to parietal cell hyperplasia causing
cellular protrusion into the glandular lumen leading to narrowing
of the glandular lumen and cystic dilation of the gland. Thus it
was proposed that FGPs occur due to mechanistic impairment
of glandular flow.[81] Dysplasia is very rare to occur in these
lesions. However the incidence and natural history of these
lesions has not been studied properly.
In community health record based studies investigating
the relationship between PPI usage and the risk of gastric
cancer, an increased risk of gastric cancer associated with PPI
use beyond the first year of treatment was reported.[82,83] However
analysis of these data indicated that the observed risk of gastric
cancer was because of confounding by indication rather than
a causal relationship with PPI use. In another prospective,
population-based cohort study, the risk estimates for gastric
cancer among PPI users was found to be close to unity after
incorporating a 1-year lag time within the diagnosis of gastric
cancer, in contrast to a substantially increased overall incidence
of gastric cancer among PPI users in analysis without lag time.[84]
Confounding by indication was again found to be one of the
main limiations of this study. In view of these limitations, the
relationship between PPI usage and development of gastric
cancer is not clear and larger studies of long-term PPI usage
are needed to clarify this issue.
Though hypergastrinemia was found to be associated with
an increased risk of colorectal carcinoma in a nested case control
study,[85] several subsequently performed population based
studies demonstrated no association between the long term
usage of PPIs and the risk of development of colorectal
cancer.[86,87,88] Regarding pancreatic cancer, no specific studies
have been done to investigate the relationship between chronic
usage of PPIs and the risk of development of pancreatic cancer.
Conclusion
PPIs in general have been reported to have low risk of serious
adverse events. There have been concerns regarding some
clinically important side effects recently and these have been
reviewed in detail. Though there is a biologically plausible
explanation for a possible interaction of PPIs with clopidogrel
which can lead to potential thrombotic risks, such a negative
interaction causing clinically meaningful outcomes has not been
consistently demonstrated in clinical studies especially in
prospective studies. A modest increase in the risk of
osteoporotic fractures and the risk of infections such as C
difficile diarrhoea, other enteric infections and pneumonia has
been found. There has been reassuring data regarding the safety
concerns of usage of PPIs in pregnancy. The results regarding
interference of PPIs with absorption of B12 and iron have been
inconsistent. There have been sporadic reports of association
of PPIs with acute interstitial nephritis and hypomagnesaemia.
Hypergastrinemia due to acid suppression by PPIs has been
shown to be associated with occurrence of benign fundic gland polyps, however the risk of gastric cancer is not clear and no
association has been found with colon cancer.
References
- Ntaios G, Chatzinikolaou A, Kaiafa G, Savopoulos C, Hatzitolios A, Karamitsos D. Evaluation of use of proton pump inhibitors in Greece. Eur J Intern Med. 2009;20:171–3.
- Eid SM, Boueiz A, Paranji S, Mativo C, Landis R, Abougergi MS. Patterns and predictors of proton pump inhibitor overuse among academic and non-academic hospitalists. Intern Med.
2010;49:2561–8.
- Ramirez E, Lei SH, Borobia AM, Piñana E, Fudio S, Muñoz R, et
al. Overuse of PPIs in patients at admission, during treatment, and at discharge in a tertiary Spanish hospital. Curr Clin Pharmacol. 2010;5:288–97.
- Ahrens D, Chenot JF, Behrens G, Grimmsmann T, Kochen MM.
Appropriateness of treatment recommendations for PPI in hospital discharge letters. Eur J Clin Pharmacol. 2010;66:1265–71.
- Craig DG, Thimappa R, Anand V, Sebastian S. Inappropriate
utilization of intravenous proton pump inhibitors in hospital practice - a prospective study of the extent of the problem and predictive factors. Q J Med. 2010;103:327–35.
- Wilde MI, McTavish D. Omeprazole. An update of its pharmacology and therapeutic use in acid-related disorders. Drugs. 1994;48:91–132.
- Benet LZ, Zech K. Pharmacokinetics - a relevant factor for the choice of a drug? Aliment Pharmacol Ther. 1994;8:25–32.
- Fitton A, Wiseman L. Pantoprazole. A review of its
pharmacological properties and therapeutic use in acid-related Proton Pump Inhibitors 181 disorders. Drugs. 1996;51:460–82.
- Langtry HD, Wilde MI. Lansoprazole. An update of its pharmacological properties and clinical effcacy in the management of acid-related disorders. Drugs. 1997;54:473–500.
- Laine L, Ahnen D, McClain C, Solcia E, Walsh JH. Review article:
potential gastrointestinal effects of long-term acid suppression with proton pump inhibitors. Aliment Pharmacol Ther. 2000;14:651–68.
- Gilard M, Arnaud B, Le Gal G, Abgrall JF, Boschat J. Influence of omeprazol on the antiplatelet action of clopidogrel associated to aspirin. J Thromb Haemost. 2006;4:2508–9.
- Gilard M, Arnaud B, Cornily JC, Le Gal G, Lacut K, Le Calvez
G, et al. Influence of omeprazole on the antiplatelet action of
clopidogrel associated With aspirin: the randomized, double-blind OCLA (Omeprazole CLopidogrel Aspirin) study. J Am Coll Cardiol. 2008;51:256–60.
- Sibbing D, Morath T, Stegherr J, Braun S, Vogt W, Hadamitzky M, et al. Impact of proton pump inhibitors on the antiplatelet effects of clopidogrel. Thromb Haemost. 2009;101:714–9.
- Cuisset T, Frere C, Quilici J, Poyet R, Gaborit B, Bali L, et al.
Comparison of omeprazole and pantoprazole influence on a high
150-mg clopidogrel maintenance dose the PACA (Proton Pump Inhibitors And Clopidogrel Association) prospective randomized study. J Am Coll Cardiol. 2009;54:1149–53.
- Furuta T, Iwaki T and Umemura K. Inûuences of different proton
pump inhibitors on the anti-platelet function of clopidogrel in relation to CYP2C19 genotypes. Br J Clin Pharmacol. 2010;70:383–92.
- Lima JP and Brophy JM. The potential interaction between
clopidogrel and proton pump inhibitors: a systematic review. BMC Medicine. 2010;8:81–9.
- Siller-Matula JM, Jilma B, Schrör K, Christ G, Huber K. Effect
of proton pump inhibitors on clinical outcome in patients treated with clopidogrel: a systematic review and meta-analysis. J Thromb Haemost. 2010;8:2624–41.
- Bhatt DL, Cryer BL, Contant CF, Cohen M, Lanas A, Schnitzer
TJ, et al (Cogent investigators). Clopidogrel with or without omeprazole in coronary artery disease. N Engl J Med. 2010;363:1909–17.
- Bo-Linn GW, Davis GR, Buddrus DJ, Morawski SG, Santa
Ana C, Fordtran JS. An evaluation of the importance of gastric acid secretion in the absorption of dietary calcium. J Clin Invest. 1984;73:640–7.
- Sheikh MS, Santa Ana CA, Nicar MJ, Schiller LR, Fordtran JS.
Gastrointestinal absorption of calcium from milk and calcium salts. N Engl J Med. 1987;317:532–6.
- Graziani G, Como G, Badalamenti S, Finazzi S, Malesci A, Gallieni
M, et al. Effect of gastric acid secretion on intestinal phosphate and calcium absorption in normal subjects. Nephrol Dial Transplant. 1995;10:1376–80.
- Serfaty-Lacrosniere C, Wood RJ, Voytko D, Saltzman JR, Pedrosa
M, Sepe TE, et al. Hypochlorhydria from short-term omeprazole
treatment does not inhibit intestinal absorption of calcium, phosphorus, magnesium or zinc from food in humans. J Am Coll Nutr. 1995;14:364–8.
- O’ Connell MB, Madden DM, Murray AM, Heaney RP, Kerzner
LJ. Effects of proton pump inhibitors on calcium carbonate absorption in women: a randomized crossover trial. Am J Med. 2005;118:778–81.
- Eastell R, Vieira NE, Yergey AL, Wahner HW, Silverstein MN, Kumar R, et al. Pernicious anaemia as a risk factor for osteoporosis. Clin Sci (Lond). 1992;82:681–5.
- Sarges R, Gallagher A, Chambers TJ, Yeh LA. Inhibition of bone resorption by H+/K(+)-ATPase inhibitors. J Med Chem.
1993;36:2828–30.
- Yang YX, Lewis JD, Epstein S, Metz DC. Long-term proton pump inhibitor therapy and risk of hip fracture. JAMA. 2006;296:2947–53.
- Vestergaard P, Rejnmark L, Mosekilde L. Proton pump inhibitors, histamine H2 receptor antagonists, and other antacid medications and the risk of fracture. Calcif Tissue Int. 2006;79:76–83.
- Kwok CS, Yeong JK, Loke YK. Meta-analysis: Risk of fractures with acid-suppressing medication. Bone. 2011;48:768–76.
- Yu EW, Bauer SR, Bain PA. Proton Pump Inhibitors and Risk of Fractures: A Meta-Analysis of 11 International Studies. Am J Med. 2011;124:519–26.
- Patel TA, Abraham P, Ashar VJ, Bhatia SJ, Anklesaria PS. Gastric bacterial overgrowth accompanies profound acid suppression. Indian J Gastroenterol. 1995;14:134–6.
- Thorens J, Froehlich F, Schwizer W, Saraga E, Bille J, Gyr K, et
al. Bacterial overgrowth during treatment with omeprazole compared with cimetidine: a prospective randomised double blind study. Gut. 1996;39:54–9.
- Williams C. Occurrence and significance of gastric colonization during acid-inhibitory therapy. Best Pract Res Clin Gastroenterol. 2001;15:511–21.
- Laheij RJ, Sturkenboom MC, Hassing RJ, Dieleman J, Stricker BH, Jansen JB. Risk of community-acquired pneumonia and use of gastric acid-suppressive drugs. JAMA. 2004;292:1955–60.
- Johnstone J, Nerenberg K, Loeb M. Meta-analysis: proton pump inhibitor use and the risk of community-acquired pneumonia. Aliment Pharmacol Ther. 2010;31:1165–77.
- Herzig SJ, Howell MD, Ngo LH, Marcantonio ER. Acidsuppressive
medication use and the risk for hospital-acquired pneumonia. JAMA. 2009;301:2120–8.
- Poutanen SM, Simor AE. Clostridium difûcile-associated diarrhea in adults. CMAJ. 2004;171:51–8.
- Verma P, Makharia GK. Clostridium difficile associated diarrhea: new rules for an old game. Tropical Gastroenterol. 2011;32:15–24.
- Al-Tureihi FI, Hassoun A, Wolf-Klein G, Isenberg H. Albumin,
length of stay, and proton pump inhibitors: key factors in Clostridium difficile-associated disease in nursing home patients. J Am Med Dir Assoc. 2005;6:105–8.
- Cunningham R, Dale B, Undy B, Gaunt N. Proton pump inhibitors as a risk factor for Clostridium difficile diarrhoea. J Hosp Infect. 2003;54:243–5.
- Dalton BR, Lye-Maccannell T, Henderson EA, Maccannell DR,
Louie TJ. Proton pump inhibitors increase signiûcantly the risk of Clostridium difficile infection in a low-endemicity, non-outbreak hospital setting. Aliment Pharmacol Ther. 2009;29:626–34.
- Yearsley KA, Gilby LJ, Ramadas AV, Kubiak EM, Fone DL,
Allison MC. Proton pump inhibitor therapy is a risk factor for Clostridium difficile-associated diarrhoea. Aliment Pharmacol Ther. 2006;24:613–9.
- Dial S, Delaney JAC, Barkun AN, Suissa S. Use of gastric acidsuppressive
agents and the risk of community-acquired Clostridium difficile-associated disease. JAMA. 2005;294:2989–95.
- Dial S, Delaney JA, Schneider V, Suissa S. Proton pump inhibitor
use and risk of community-acquired Clostridium difficileassociated disease defined by prescription for oral vancomycin therapy. CMAJ. 2006;175:745–8.
- Jump RL, Pultz MJ, Donskey CJ. Vegetative Clostridium difficile
survives in room air on moist surfaces and in gastric contents with elevated pH. Antimicrob Agents Chemother. 2007;51:2883–7.
- Pepin J, Saheb N, Coulombe MA, Alary ME, Corriveau MP,
Authier S, et al. Emergence of fluoroquinolones as the predominant
risk factor for Clostridium difficile-associated diarrhea: a cohort study during an epidemic in Quebec. Clin Infect Dis. 2005;41:1254–60.
- Shah S, Lewis A, Leopold D, Dunstan F, Woodhouse K. Gastric acid suppression does not promote clostridial diarrhoea in the elderly. Q J Med. 2000;93:175–81.
- Wilcox MH, Mooney L, Bendall R, Settle CD, Fawley WN. A case-control study of community-associated Clostridium difficile infection. J Antimicrob Chemother. 2008;62:388–96.
- Leonard J, Marshall JK, Moayyedi P. Systematic review of the risk of enteric infection in patients taking acid suppression. Am J Gastroenterol. 2007;102:2047–56.
- Howell MD, Novack V, Grgurich P, Soulliard D, Novack L,
Pencina M, et al. Iatrogenic gastric acid suppression and the risk of nosocomial Clostridium difficile infection. Arch Intern Med. 2010;170:784–90.
- Nerandzic MM, Pultz MJ, Donskey CJ. Examination of potential
mechanisms to explain the association between proton pump inhibitors and Clostridium difficile infection. Antimicrob Agents Chemother. 2009;53:4133–7.
- Gill SK, O’Brien L, Einarson TR, Koren G. The safety of proton pump inhibitors (PPIs) in pregnancy: a meta-analysis. Am J Gastroenterol. 2009;104:1541–5.
- Pasternak B, Hviid A. Use of proton-pump inhibitors in early pregnancy and the risk of birth defects. N Engl J Med. 2010;363:2114–23.
- Sierra F, Suarez M, Rey M, Vela MF. Systematic review: Proton pump inhibitor-associated acute interstitial nephritis. Aliment Pharmacol Ther. 2007;26:545–53.
- Festen HP. Intrinsic factor secretion and cobalamin absorption: Physiology and pathophysiology in the gastrointestinal tract. Scand J Gastroenterol Suppl. 1991;188:1–7.
- Saltzman JR, Kemp JA, Golner BB, Pedrosa MC, Dallal GE,
Russell RM. Effect of hypochlorhydria due to omeprazole treatment or atrophic gastritis on protein-bound vitamin B12 absorption. J Am Coll Nutr. 1994;13:584–91.
- Marcuard SP, Albernaz L, Khazanie PG. Omeprazole therapy causes malabsorption of cyanocobalamin (vitamin B12). Ann Intern Med. 1994;120:211–5.
- Schenk BE, Festen HP, Kuipers EJ, Klinkenberg-Knol EC,
Meuwissen SG. Effect of short- and long-term treatment with omeprazole on the absorption and serum levels of cobalamin. Aliment Pharmacol Ther. 1996;10:541–5.
- Kittang E, Aadland E, Schjonsby H, Rohss K. The effect of omeprazole on gastric acidity and the absorption of liver cobalamins. Scand J Gastroenterol. 1987;22:156–60.
- Valuck RJ, Ruscin JM. A case-control study on adverse effects: H2 blocker or proton pump inhibitor use and risk of vitamin B12 deficiency in older adults. J Clin Epidemiol. 2004;57:422–8.
- Termanini B, Gibril F, Sutliff VE, Yu F, Venzon DJ, Jensen RT.
Effect of long-term gastric acid suppressive therapy on serum vitamin B12 levels in patients with Zollinger-Ellison syndrome. Am J Med. 1998;104:422–30.
- den Elzen WP, Groeneveld Y, de Ruijter W, Souverijn JH, le
Cessie S, Assendelft WJ, et al. Long-term use of proton pump inhibitors and vitamin B12 status in elderly individuals. Aliment Pharmacol Ther. 2008;27:491–7.
- Quamme GA. Recent developments in intestinal magnesium absorption. Curr Opin Gastroenterol. 2008;24:230–5.
- Mackay JD, Bladon PT. Hypomagnesaemia due to proton-pump inhibitor therapy: a clinical case series. QJM. 2010;103:387–95.
- Cundya T, Mackay J. Proton pump inhibitors and severe hypomagnesaemia. Curr Opin Gastroenterol. 2011;27:180–5.
- Jeppesen PB, Staun M, Tjellesen L, Mortensen PB. Effect of
intravenous ranitidine and omeprazole on intestinal absorption of water, sodium, and macronutrients in patients with intestinal resection. Gut. 1998;43:763–9.
- Serfaty-Lacrosniere C, Wood RJ, Voytko D, Saltzman JR, Pedrosa
M, Sepe TE, et al. Hypochlorhydria from short-term omeprazole
treatment does not inhibit intestinal absorption of calcium, phosphorus, magnesium or zinc from food in humans. J Am Coll Nutr. 1995;14:364–8.
- Bezwoda W, Charlton R, Bothwell T, Torrance J, Mayet F. The importance of gastric hydrochloric acid in the absorption of nonheme food iron. J Lab Clin Med. 1978;92:108–16.
- Koop H, Bachem MG. Serum iron, ferritin, and vitamin B12 during prolonged omeprazole therapy. J Clin Gastroenterol. 1992;14:288–92.
- Stewart CA, Termanini B, Sutliff VE, Serrano J, Yu F, Gibril F, et
al. Iron absorption in patients with Zollinger-Ellison syndrome treated with long-term gastric antisecretory therapy. Aliment Pharmacol Ther. 1998;12:83–98.
- Hutchinson C, Geissler CA, Powell JJ, Bomford A. Proton pump inhibitors suppress absorption of dietary non-haem iron in hereditary haemochromatosis. Gut. 2007;56:1291–5.
- Dockray GJ, Varro A, Dimaline R, Wang T. The gastrins: their production and biological activities. Annu Rev Physiol. 2001;63:119–39.
- Noble F, Wank SA, Crawley JN, Bradwejn J, Seroogy KB, Hamon
M, et al. International Union of Pharmacology. XXI. Structure, distribution and functions of cholecystokinin receptors. Pharmacol Rev. 1997;51:745–81.
- Miyake A, Mochizuki S, Kawashima H. Characterization of cloned human cholecystokinin-B receptor as a gastrin receptor. Biochem Pharmacol. 1994;47:1339–43.
- Guo YS, Townsend CM Jr. Role of gastrointestinal hormones in pancreatic cancer. J Hepatobiliary Pancreat Surg. 2000;7:276–85.
- McWilliams DF, Watson SA, Crosbee DM, Michaeli D, Seth R.
Coexpression of gastrin and gastrin receptors (CCK-B and delta CCK-B) in gastrointestinal tumour cell lines. Gut. 1998;42:795–8.
- Smith JP, Stanley WB, Verderame MF, Zagon IS. The functional signiûcance of the cholecystokinin-C (CCK-C) receptor in human pancreatic cancer. Pancreas. 2004;29:271–7.
- Seva C, Dickinson C, Yamada T. Growth-promoting effects of glycine-extended progastrin. Science. 1994;265:410–2.
- Kochman ML, DelValle J, Dickinson CJ, Boland CR. Posttranslation processing of gastrin in neoplastic human colonic tissues. Biochem Biophys Res Commun. 1992;189:1165–9.
- Larsson H, Carlsson E, Hakanson R, Mattsson H, Nilsson G,
Seensalu R, et al. Time-course of development and reversal of
gastric endocrine cell hyperplasia after inhibition of acid secretion. Studies with omeprazole and ranitidine in intact and antrectomized rats. Gastroenterol. 1988;95:1477–86.
- Klinkenberg-Knol EC, Nelis F, Dent J, Snel P, Mitchell B, Prichard
P, et al. Long-term omeprazole treatment in resistant gastroesophageal reflux disease: efficacy, safety and influence on gastric mucosa. Gastroenterol. 2000;118:661–9.
- Cats A, Schenk BE, Bloemena E, Roosedaal R, Lindeman J,
Biemond I, et al. Parietal cell protrusions and fundic gland cysts during omeprazole maintenance treatment. Hum Pathol. 2000;31:684–90.
- Bateman DN, Colin-Jones D, Hartz S, Langman M, Logan RF, Mant J, et al. Mortality study of 18 000 patients treated with omeprazole. Gut. 2003;52:942–6.
- Garcia Rodriguez LA, Lagergren J, Lindblad M. Gastric acid suppression and risk of oesophageal and gastric adenocarcinoma: a nested case control study in the UK. Gut. 2006;55:1538–44.
- Poulsen AH, Christensen S, McLaughlin JK, Thomsen RW,
Sorensen HT, Olsen JH, et al. Proton pump inhibitors and risk of gastric cancer: a population-based cohort study. Br J Cancer. 2009;100:1503–7.
- Thorburn CM, Friedman GD, Dickinson CJ, Vogelman JH, Orentreich N, Parsonnet J. Gastrin and colorectal cancer: a prospective study. Gastroenterol. 1998;115:275–80.
- Yang YX, Hennessy S, Propert K, Hwang WT, Sedarat A, Lewis JD. Chronic proton pump inhibitor therapy and the risk of colorectal cancer. Gastroenterol. 2007;133:748–54.
- van Soest EM, van Rossum LGM, Dieleman JP, van Oijen MG,
Siersema PD, Sturkenboom MC, et al. Proton pump inhibitors and the risk of colorectal cancer. Am J Gastroenterol. 2008;103:966–73.
- Robertson DJ, Larsson H, Friis S, Pedersen L, Baron JA, Sorensen HT. Proton pump inhibitor use and risk of colorectal cancer: a population-based, case-control study. Gastroenterol.
2007;133:755–60.