48uep6bbphidvals|445
48uep6bbph|2000F98CTab_Articles|Fulltext
Congenital absence of the portal vein (CAPV) is a rare anomaly
in which portal venous blood bypasses the liver through a
congenital portosystemic shunt.[1,2,3,4,5,6,7,8,9,10,11] The drainage sites of portal
venous blood include the inferior vena cava (IVC), the left
renal vein and less commonly the internal iliac vein, azygosvein and right atrium.[1,2,3,4,5,6,7,8,9,10,11] Although the portosystemic shunt
may be accompanied by hyperammonemia, hyperbilirubinemia
and hypergalactosemia; hyperinsulinemia and
hyperandrogenism have rarely been reported in patients with
CAPV.[1,12] To the best of our knowledge, only three cases of
congenital extrahepatic portosystemic shunts with
hyperinsulinemia and hyperandrogenism have been
reported.[5,12] We report a case of CAPV associated with large
inferior mesenteric-caval shunt in a 20 year old female with
hyperinsulinemia and hyperandrogenism.
Case report
A 20 year old female presented to our hospital with history of
rectal bleeding since 5 years of age. She required multiple blood
transfusions because of chronic rectal bleeding and severe
anemia. She underwent hemorrhoidectomy thrice in past
without any significant relief in the symptoms. No significant
family history was present. The patient had primary
amenorrhoea and signs of secondary virilization including
clitoromegaly. On examination, breast development was normal
(Tanner stage 4). There were excessive hairs over the face and
back. Neurological examination was normal and there were no
manifestation of hepatic encephalopathy.
Liver function tests revealed normal levels of transaminase,
alkaline phosphate and bilirubin. Serological markers for
hepatitis B and C were negative and serum ammonia levels
were normal (48 µg/dl). Serum FSH, LH and estradiol were within
normal range. Oral glucose tolerance test revealed
hyperglycemia and hyperinsulinemia indicating insulin
insensitivity. Serum testosterone levels were 1.49 ng/ml (normal
range: 0.05-0.73 ng/ml), and dehydroepiandosterone (DHEA)
level was 6.5 ng/ml.
Ultrasound revealed absence of the portal vein. The right
lobe of the liver was hypoplastic and there was no focal lesion.
However, ultrasound failed to demonstrate the anatomy of extra
hepatic portosystemic shunt. Ultrasound pelvis revealed
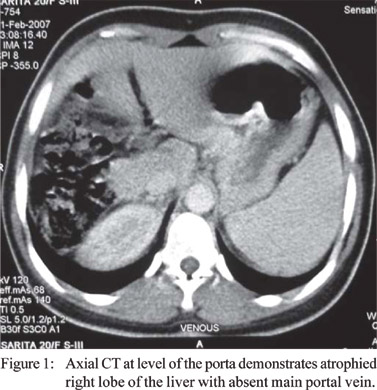
normal sized uterus and enlarged ovaries. CECT of the abdomen
revealed normal hepatic veins and absence of intrahepatic portal
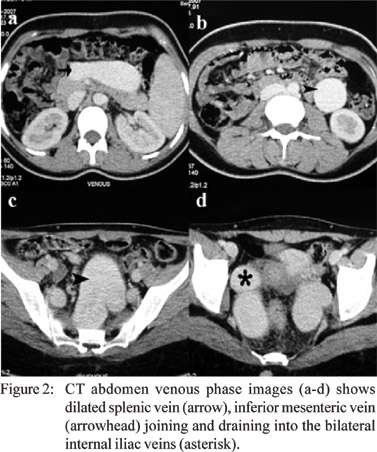
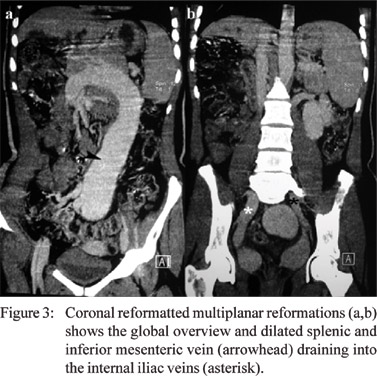
vein (Figure 1). A markedly dilated inferior mesenteric vein
was seen draining into the internal iliac veins (Figure 2, 3).
Celiac axis and superior mesenteric artery were normal. Spleen
was normal in size and there were no portosystemic collaterals.
Echocardiography was normal.
A diagnosis of the congenital absence of the portal vein
associated with large inferior mesenteric-caval shunt causing
hyperinsulinemia and hyperandrogenism was made. The patient
was started on the cyclic oestrogen and her menstrual cycles
started.
Discussion
Congenital absence of the portal vein (CAPV), a subtype of
congenital portosystemic shunt is a rare anomaly with only
few cases reported in the literature.[1,2,3,4,5,6,7,8,9,10,11] Abernethy malformation
in which there is congenital diversion of the blood away from
the liver was first reported in 1793. Morgan and Superina[13]
classified congenital extra hepatic portosystemic shunts in two
types: type 1 (side to end anastomosis) or congenital absence
of the portal vein occurs predominately in females and is
associated with multiple malformations; and Type II (side to
side anastomosis) in which portal vein supply is partially
preserved and have no sex predisposition and associated
malformations.
In CAPV the intestinal and splenic venous drainage
bypasses the liver and drains directly into the systemic veins.[13]
CAPV is further classified into two types based on the anatomy
of the portal vein. In type A, the superior mesenteric vein and
splenic vein do not join and drain separately into systemic
veins. In type B, the superior mesenteric vein and the splenic
vein join before draining into systemic vein. Drainage sites
include inferior vena cava (IVC), the left renal vein and less
commonly the internal iliac vein, azygos vein and right atrium.
The present case corresponds to type B.
CAPV with large inferior mesenteric–iliac vein shunt is
uncommon since shorter tracts (splenorenal, superior
mesenteric-caval) are utilized in preference to this long venous
channel. CAPV results from aberration in venous development in
early embryonic life. Embryologically, portal vein develops from
selective involution of right and left vitelline veins and their
medial anastomosis during second month of gestation.
Excessive involution results in absence of the portal vein.
Development of inferior vena cava in close proximity of the
portal vein and during same time period likely explains the
basis of congenital extra hepatic portosystemic shunts.[3,6]
The age of diagnosis of CAPV ranges from 1 day to 64
years. However, they predominantly occur in females and
children.[1,2,3,4,5,6,7,8,9,10,11] Extrahepatic portosystemic shunt occurs without
secondary signs of portal hypertension, such as venous
collateral, ascites, and splenomegaly. Liver function tests and
ammonia levels are either normal or mildly elevated. Clinical
presentation is variable and reported presentations include
hypergalactosemia, hyperammonemia, hyperbilirubinemia, liver
mass, mental retardation, amenorrhea and hemorrhoidal
bledding.1-12 Our case presented with complaints of
hemorrhoidal bleeding and amenorrhea.
Hyperinsulinemia in congenital portosystemic shunt is
secondary to increased production and reduced clearance of
the insulin. Production increases because of impaired glucose
utilization by liver secondary to reduced supply of insulin and
glucose from portal vein. Portal blood bypasses the liver, thus
reducing the clearance of insulin. Satoh et al[12] postulated that
hyperinsulinemia in congenital portosystemic shunt leads to
hyperandrogenism akin to insulin resistance states like
polycystic ovary syndrome and insulin resistance diabetes
mellitus.
Congenital absence of the portal vein is usually associated
with other congenital abnormalities[1,10,14] including
cardiovascular (dextrocardia, ventricular or atrial septal defects,
patent foramen ovale and ductus arteriosus); skeletal
(hemivertebrae, oculoauriculovertebral dysplasia); and biliary
(biliary atresia). None of these congenital malformations was
present in the present case. Liver neoplasm (focal nodular
hyperplasia, adenoma, hepatoblastoma, HCC) are also
frequently associated with CAPV.[14] No hepatic lesion was
identified in our patient.
The right lobe of liver was hypoplastic in the present case.
Similarly hypoplastic right lobe and small liver volumes was
reported by Goo et al.[8] The authors postulated that hypoplasia
might have resulted from insufficient supply of hepatotrophic
substance to the liver. Liver transplantation is the only effective
treatment for CAPV.
References
- Hu GH, Shen LG, Yang J, Mei JH, Zhu YF. Insight into congenital
absence of the portal vein: is it rare? World J Gastroenterol.
2008;14:5969–79.
- Gallego C, Miralles M, Marin C, Muyor P, Gonzalez G, Garcia-
Hidalgo E. Congenital hepatic shunts. Radiographics.
2004;24:755–72.
- Komatsu S, Nagino M, Hayakawa N, Yamamoto H, Nimura Y.
Congenital absence of portal venous system associated with a
large inferior mesenteric-caval shunt: a case report.
Hepatogastroenterology. 1995;42:286–90.
- Arana E, Marti-Bonmati L, Martinez V, Hoyos M, Montes H.
Portal vein absence and nodular regenerative hyperplasia of the
liver with giant inferior mesenteric vein. Abdom Imaging.
1997;22:506–8.
- Grazioli L, Alberti D, Olivetti L, Rigamonti W, Codazzi F,
Matricardi L, et al. Congenital absence of portal vein with nodular
regenerative hyperplasia of the liver. Eur Radiol. 2000;10:820–5.
- Niwa T, Aida N, Tachibana K, Shinkai M, Ohhama Y, Fujita K, et
al. Congenital absence of the portal vein: clinical and radiologic
findings. J Comput Assist Tomogr. 2002;26:681–6.
- Turkbey B, Karcaaltincaba M, Demir H, Akcoren Z, Yuce A,
Haliloglu M. Multiple hyperplastic nodules in the liver with
congenital absence of portal vein: MRI findings. Pediatr Radiol.
2006;36:445–8.
- Goo HW. Extrahepatic portosystemic shunt in congenital absence of the portal vein depicted by time-resolved contrast-enhanced MR angiography. Pediatr Radiol. 2007;37:706-9.
- Takagaki K, Kodaira M, Kuriyama S, Isogai Y, Nogaki A, Ichikawa
N, et al. Congenital absence of the portal vein complicating hepatic
tumors. Intern Med. 2004;43:194–8.
- De Gaetano AM, Gui B, Macis G, Manfredi R, Di Stasi C.
Congenital absence of the portal vein associated with focal nodular
hyperplasia in the liver in an adult woman: imaging and review of
the literature. Abdom Imaging. 2004;29:455–9.
- Kawano S, Hasegawa S, Urushihara N, Okazaki T, Yoshida A,
Kusafuka J, et al. Hepatoblastoma with congenital absence of the
portal vein - a case report. Eur J Pediatr Surg. 2007;17:292–4.
- Satoh M, Yokoya S, Hachiya Y, Hachiya M, Fujisawa T, Hoshino
K, Saji T. Two hyperandrogenic adolescent girls with congenital
portosystemic shunt. Eur J Pediatr. 2001;160:307–11.
- Morgan G, Superina R. Congenital absence of the portal vein:
two cases and a proposed classification system for portasystemic
vascular anomalies. J Pediatr Surg. 1994;29:1239–41.
- Pichon N, Maisonnette F, Pichon-Lefièvre F, Valleix D, Pillegand
B. Hepatocarcinoma with congenital agenesis of the portal vein.
Jpn J Clin Oncol. 2003;33:314–6.