48uep6bbphidvals|447
48uep6bbph|2000F98CTab_Articles|Fulltext
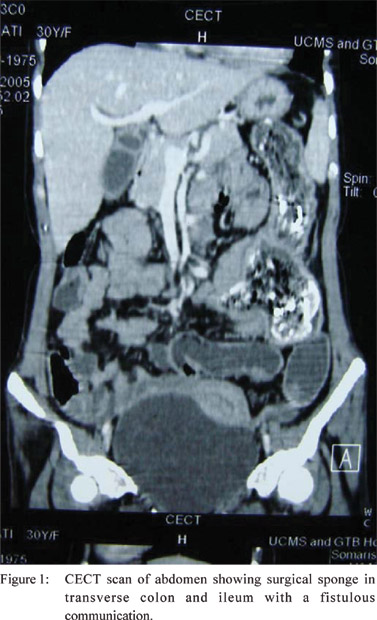
Case 1
A 30 year old woman presented with pain and lump in left lower
abdomen of two years duration. She had undergone caesarean
section two years back. Examination revealed pallor and an
intra-abdominal, nontender, firm, irregular lump measuring 10 ×
8 cms with restricted mobility in the left lower abdomen.
Laboratory investigations revealed microcytic hypochromic
anemia. Ultrasonography (USG) of the abdomen was
unremarkable. Contrast enhanced CT (CECT) scan of the
abdomen showed a segment of transverse colon adherent to
ileum with surrounding inflammation. An intraluminal, irregular,
calcified mass in the adherent segments of the bowel was seen
incorporating a tortuous, linear, radiopaque density suggestive
of retained surgical sponge (Figure 1).
On laparotomy, a segment of distal ileum was found adherent
to transverse colon. The serosal surfaces of bowel were normal.
There was no ascites, lymphadenopathy, peritoneal deposits
or hepatic metastasis. Involved segments of ileum and
transverse colon were resected and gut continuity was restored
by ileo-ileal and colo-colic anastomosis. On opening the
resected specimen a surgical sponge lying in the lumen of the
ileum and extending into the transverse colon through a
fistulous communication was found. The patient made a good
post-operative recovery and was discharged on 8th postoperative
day.
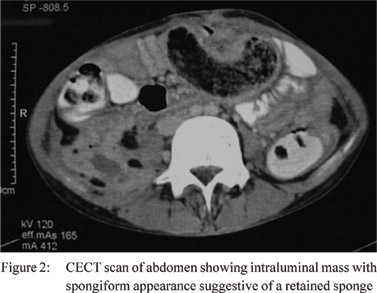
Case 2
A 16-year-old boy presented with colicky abdominal pain and
bilious vomiting for 4 days. He had undergone laparotomy for
duodenal ulcer perforation 3 months back. General physical
examination was unremarkable except for dehydration.
Abdomen was not distended, scar of the previous surgery
was healthy and visible peristalsis was present. A 4 × 6 cm
firm, tender lump, moving with respiration and with a dull
percussion note was found in the left upper abdomen. Bowel
sounds were exaggerated. Laboratory investigations and Xray
of the abdomen were unremarkable. USG of abdomen
showed dilated bowel loops with hyper echoic mass in the left
lumbar region. CECT scan of the abdomen showed a mass
with spongiform appearance suggestive of a retained sponge
(Figure 2). Laparotomy revealed distended jejunal loops
proximal to a palpable mass inside the bowel lumen about 1½
foot distal to duodenojejunal flexure. The serosal surfaces of the bowel were normal and distal bowel loops were collapsed.
Enterotomy revealed a retained surgical sponge which was
retrieved and enterotomy incision closed primarily. The patient
made an uneventful recovery.
Discussion
Retained foreign bodies (FB) constitute a mishap in modern
surgery. Most common among these is an accidentally
overlooked surgical sponge.[5] Retained surgical sponge is also
known as gossypiboma [Gossypium (Latin): cotton; oma
(Kiswahili): place of concealment][2], textiloma[1] and cottonoid.
Exact incidence of gossypiboma is unknown as the condition
is considered to be widely underestimated and under reported,
possibly due to fear of medicolegal implications.[1,2,6,7,8] Reported
incidence varies from 1 in 100-3000 for all surgical interventions,
and 1 in 1000-1500 for intra-abdominal operations.[1,2,6]
Gossypiboma has been reported following gynecological,
abdominal, cardiothoracic, orthopedic, and neurosurgical
procedures.[[1,6,9]
The clinical presentation of patients with gossypiboma is
varied which causes considerable diagnostic dilemma.[1] Its
presence should be suspected in any patient where the postoperative
recovery was not smooth or re-admission was
required for persistent symptoms.[6] Gossypiboma may cause
bowel obstruction, perforation, granulomatous peritonitis,
septic syndrome, fistulization to the neighboring organs, or
may mimic a chronic inflammatory process like tuberculosis[10]
and even malignancy.[1,2,11] At times it may be lethal,[3,6] however
it may remain asymptomatic for years.[1,6] Rarely gossypiboma
may migrate to the neighboring organs due to persistent
pressure and subsequent erosion through their wall.[2,3,4] Intestine is the commonest organ where migration occurs, as seen with
both of our patients. This is attributed to the large surface area
and relatively thin wall of the intestine which provides least
resistance to their transmural migration. Other organs where
such migration, although uncommon, has been reported include
urinary bladder, stomach and thorax (through diaphragm).[1]
Radiological features of gossypibomas are variable.
Detection by plain X-ray is difficult,[11] especially when surgical
sponges have not been provided with the radiopaque marker
or when the marker has been fragmented or disintegrated, the
presence of which may aid in diagnosis.[2,6,7] USG may be helpful
and may show an echogenic, complex hypoechoic area, or
cystic mass with acoustic shadow or may be normal[1,12] . CECT
scan is the investigation of choice.[13,14] It may show complex
mass with variable density; calcification; spongiform gas and
radiopaque marker 1(if present), as was seen in patient [1]. In
patient [2], since the sponge lacked a radiopaque marker it was
not visible on radiological investigations. MRI is also
infrequently used for diagnosis.[7] Once diagnosed,
gossypibomas require removal, as morbidity and complications
associated with it are high.[1,2] This usually necessitates
laparotomy. However, alternative methods like laparoscopy,
percutaneous extraction (with or without the help of
interventional radiology)9 and endoscopic procedures have
been reported.[12] Spontaneous extrusion is an extremely rare
favorable outcome.[1,7]
Risk factors leading to gossypiboma include a higher mean
body-mass index, emergency surgery, difficult operative
procedure, surgeon’s fatigue, several sponges sticking
together, poor tracking, change in nursing and surgical teams,
an unplanned change in the operation and unaccountable
human error.[2,12] Although importance of meticulous counting
cannot be over emphasized, cases have been reported in
presence of normal counts.[1,2] Some authors suggest routine
X-ray screening of high-risk patients before they leave the
operating room even if the count is documented to be correct,
although this has not been found to be foolproof.[1,2] thers
have suggested use of sponges held in forceps to prevent
their intra-operative loss.[8] With technological advancement,
the future holds promise for the use of hand held detectors
and scanners that will either supplement or replace manual
counting. Various other innovations like bar coding of
instruments and sponges, radiofrequency identification and
electronic surveillance systems are being developed.[15]
References
- Zantvoord Y, van der Weiden RM, van Hooff MH. Transmural
migration of retained surgical sponges: a systematic review. Obstet
Gynecol Surv. 2008;63:465–71.
- Sarda AK, Pandey D, Neogi S, Dhir U. Postoperative
complications due to a retained surgical sponge. Singapore Med
J. 2007;48:e160–4.
- Falleti J, Somma A, Baldassarre F, Accurso A, D’Ettorre
A, Insabato L. Unexpected autoptic finding in a sudden death:
gossypiboma. Forensic Sci Int. 2010;199:e23–6.
- Kansakar R, Thapa P, Adhikari S. Intraluminal migration of
Gossypiboma without intestinal obstruction for fourteen years.
JNMA J Nepal Med Assoc. 2008;47:136–8.
- Dhillon JS, Park A. Transmural migration of a retained laparotomy
sponge. Am Surg. 2002;68:603–5.
- Alis H, Soylu A, Dolay K, Kalaycý M, Ciltas A. Surgical
intervention may not always be required in gossypiboma with
intraluminal migration. World J Gastroenterol. 2007;13:6605–7.
- Godara R, Marwah S, Karwasra RK, Goel R, Sen J, Singh R.
Spontaneous transmural migration of surgical sponges. Asian J
Surg. 2006;29:44–5.
- Glockemann K, Fröhlich H, Bernhards J, Büttner D. Peranal
passage of a surgical sponge: fortunate outcome of an
intraoperative oversight. Chirurg. 2005;76:595–8.
- Rappaport W, Haynes K. The retained surgical sponge following
intra-abdominal surgery. A continuing problem. Arch Surg.
1990;125:405–7.
- Sinha SK, Gupta S, Behra A, Khaitan A, Kochhar R, Sharma
BC, et al. Retained surgical sponge: an unusual cause of
malabsorption. Trop Gastroenterol. 1999;20:42–4.
- Haddad R, Judice LF, Chibante A, Ferraz D. Migration of surgical
sponge retained at mediastinoscopy into the trachea. Interact
Cardiovasc Thorac Surg. 2004;3:637–40.
- Erdil A, Kilciler G, Ates Y, Tuzun A, Gulsen M, Karaeren N, et
al. Transgastric migration of retained intraabdominal surgical
sponge: gossypiboma in the bulbus. Intern Med. 2008;47:613–5.
- Haddad R, Judice LF, Chibante A, Ferraz D. Migration of surgical
sponge retained at mediastinoscopy into the trachea. Interact
Cardiovasc Thorac Surg. 2004;3:637–40.
- Klariæ Custoviæ R, Krolo I, Marotti M, Babiæ N, Karapanda N. Retained surgical textilomas occur more often during war.
Croat Med J. 2004;45:422–6.
- Gibbs VC. Patient safety practices in operating room: correctsite
surgery and nothing left behind. Surg Clin North Am.
2005;85:1307–19, xiii.
- Kacker R. Retained foreign bodies in the abdominal cavity. In: Roshan Lall Gupta, editors. The medicolegal aspects of Surgery. Ist ed. New Delhi: Jaypee Brothers; 1999. p.176.