Portal hypertension (PHT) induced variceal bleed is the commonest cause of upper gastrointestinal hemorrhage in children.
[1] Endoscopic and pharmacological treatment options are available for prophylaxis of first upper gastrointestinal hemorrhages in pediatric population.
[2] The efficacy of endoscopic band ligation (EVL) and endoscopic sclerotherapy (EIS) in averting esophageal variceal bleed has been proven beyond doubt.
[3,
4] The limitations however include their being invasive and expensive procedures, along with the requirement of expertise and multiple sittings. Moreover, in resource poor countries of the developing world, these therapeutic modalities are outside the reach of many, especially those from remote locations. In contrast, therapeutic drugs including beta blockers are a readily available alternative for decreasing portal venous pressure (PVP).
[5] But data regarding the use of these drugs for prophylaxis of portal hypertension hemorrhages in pediatric patients have yielded conflicting results.
[6,
7] Our purpose hence was to evaluate the efficacy of beta blockers in preventing variceal bleed in children suffering from PHT. The secondary aim was to assess whether the newer generation beta blockers were superior to conventional ones.
Methods
Our study was a randomized trial, conducted in a tertiary care hospital setting between March 2007 and February 2011. Subjects below 12 years of age were enrolled in the study over the first 2 years, on the basis of the following inclusion criteria: history and clinical features indicative of PHT, supported by information from relevant investigations (documented gastrooesophageal varices in upper gastrointestinal endoscopy along with corroborative liver function tests, suggestive Doppler ultrasound of abdomen and histopathology reports of liver biopsy wherever applicable). Children suffering from childhood asthma, juvenile diabetes mellitus or any form of cardiovascular disease were excluded. All the drop outs over the mean followup period were not incorporated in the study.
Oesophagealvarices were graded from I to IV, according to Conn's staging.
[8] Gastric varices were categorized into gastroeosophageal varices (GOV) and isolated gastric varices (IGV) as per Sarin's classification.
[9] The stomach was also screened for portal hypertensive gastropathy (PHG).
The enlisted cases were first of all assorted into groups on the basis of etiology of portal hypertension (sinusoidal or presinusoidal) and then each group was again subdivided into subgroups according to the grade of varices. All the subgroups thus created were divided by randomization into two nearly equal sets A and B. This was done using computer generated random selections to determine whether the first patient of each subgroup would be enlisted in either set A or set B. Similarly each patient from every subgroup was randomized into one of the two sets.
We limited our trial to 2 drugs, propranolol and carvedilol. Propranolol is a non selective b-blocker and has been in clinical use for quite some time for primary as well as secondary prophylaxis ofvariceal bleed, with mixed results.
[10] Carvedilol on the other hand is a relatively newer non selective b -blocker with additional a1 blocking action and has recently been used at some centers for PHT with beneficial results.
[11] In set A, children were given propranolol and in set B, subjects were administered carvedilol .The patients were initially admitted to the inpatient department of our institute and the drugs were given orally at a dose of 1mg/kg/day and 0.3 mg/kg/day, respectively. After titration of the doses to decrease the sleeping heart rate by 25%, the children were discharged.
All patients underwent surveillance endoscopy at scheduled intervals over the next 2 years. The surveillance was done at monthly intervals from second month onwards for the first 6 months. Subsequently it was done at quarterly intervals. Efficacy was defined by no episode of bleeding along with reduction of any of the three: grade of esophageal varices (on the basis of Conn's classification), severity of gastric varices (as per Sarin's classification) or PHG (on basis of subjective evaluation of the endoscopist); provided there was no increase in the grade and/or severity of the other 2 types of pathology. Those patients who had breakthrough bleeding were consequently not treated with the standard drug intervention protocol and managed with endoscopic therapy. However, they were included while analyzing their results as non responders.
The study was approved by our institutional ethics committee and each patient was enlisted after obtaining informed consent from the parent/guardian. The analysis was carried out using SPSS statistical package. A p value less than 0.05 and coefficient of correlation (r) greater than 0.5, were taken as significant. The minimal sample size needed was calculated assuming a minimum power of study of 80%.
Results
Of the 67 patients followed over a period of 2 years, 3 subjects had to be excluded. Two children suffering from chronic liver disease died during follow up, both due to hepatic decompensation. So our analysis was restricted to 62 children. The confirmed etiologies in 41 patients with sinusoidal causes included Wilson's disease (n=5), glycogen liver disorder (n=3), hepatitis B virus induced chronic liver disease (n=3), hepatitis C virus induced liver disease (n=2), Gaucher's disease (n=1), progressive familial intrahepatic cholestasis (PFIC) (n=1) and autoimmune liver disease (n=1). The remaining cases were idiopathic. All the cases presented with clinical features of chronic liver disease, either compensated or decompensated. Propranolol was prescribed in 21 children (group IA), the remaining were treated with carvedilol (group IB).
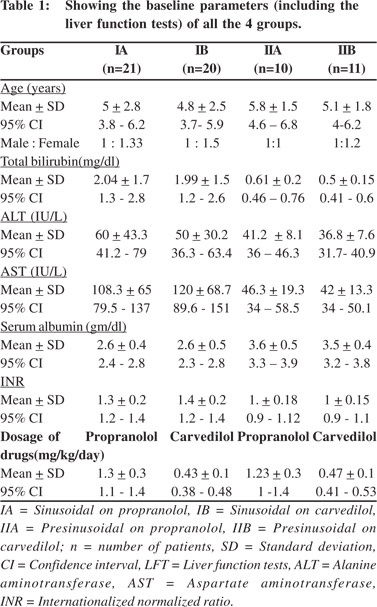
In the presinusoidal cluster of 21 cases, 6 patients were affected by noncirrhotic portal fibrosis (NCPF), 3 children had perinatal history of exchange transfusion and 3 kids had suffered from neonatal sepsis with omphalitis. One case in this group had history of acute gastroenteritis with severe dehydration leading to hospital admission in infancy. The major complaint of subjects with presinusoidal etiology was unexplained abdominal distension. In this subset, ten cases (group IIA) were managed with propranolol, and the remaining 11 patients (group IIB) with carvedilol. Table 1 shows the baseline parameters (including the liver function tests) of all the 4 groups.
At the end of 2 years follow-up, 40 patients witnessed a decrease in the grade of their oesophageal varices. In 13 children, the grade remained the same and 9 cases witnessed an increase in their grade. Of the 9 subjects with GOV, varices persisted in 6 subjects but their severity was reduced in 8 of them. There was however no substantial reduction of PHG in any of the 4 patients. None of the children had IGV neither during enrollment nor during follow-up.
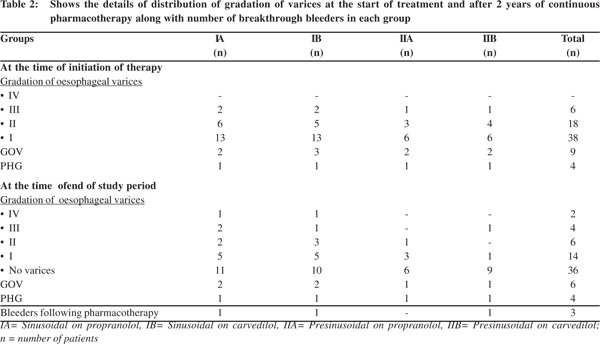
Three (4.83%) children suffered breakthrough bleeding. At the time of bleeding, patients 1 and 2 had grade IV and III varices respectively. They were consequently managed with band ligation and were put on secondary prophylaxis with b-blockers. Table 2 shows details of distribution of gradation of varices at the start of treatment and after 2 years of continuous pharmacotherapy along with number of bleeders in each group.
Hypotension (defined as SBP <5th percentile for age) was not encountered in any of the subjects. No form of cardiovascular disease, renal compromise or weight gain (>10% increase in weight over 6 months) was noted in any patient. No other commonly mentioned side effects of the drugs occurred, that would necessitate withdrawal of the drugs.
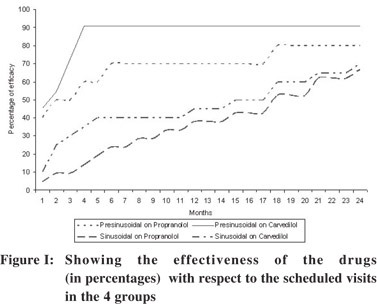
Both the drugs were statistically effective with respect to time (months), the correlation coefficient (r) being 0.99, 0.94, 0.87 and 0.57 for the groups IA, IB, IIA, and IIB, respectively. Figure 1 shows the effectiveness of the drugs (in percentages) with respect to the scheduled visits in the 4 groups. The figure highlights that for both drugs, the efficacy was higher and the response achieved much faster in children with presinusoidal etiologies than those with sinusoidal causes of PHT. It also emphasizes that carvedilol was much quicker to act in comparison to propranolol though in the long run results were near similar.
Individually, in both the sinusoidal and presinusoidal categories, the difference in efficacy of propranolol and carvedilol was insignificant (p>0.05), through all the serial visits. On the other hand, when combined the difference between the efficacy of the two drugs was significant, but only at 4 and 5 month follow-up period (p = 0.035 and p = 0.034, respectively). Assuming that for each patient the drugs were to be continued till the age of 18 years, propranolol stood out to be more cost effective (p <0.01) than carvedilol in our setting.
Discussion
Management of pediatric PHT differs in a great way from that of adults not only due to etiological divergence, but also because the pharmacokinetics and pharmacodynamics of drugs used for PHT vary considerably in children from that in adults. There have been a few studies on medical prophylaxis of first variceal bleeding by non selective b-blockers, but most were restricted to adult population, especially in cirrhotics.
[12,
13] Non selective b-blockers act a) by blocking b1 receptors and reducing the cardiac output and b) by blocking b2 receptors, producing splanchnic vasoconstriction and reducing the portal flow.
[14] Their efficacy in primary prophylaxis for moderate to large varices is well documented and their use in small varices is optional.
[15,
16] Since we dealt with a very vulnerable group of pediatric population we decided to use the drugs irrespective of the grade of varix.
We observed that in presinusoidal type of PHT, b-blockers are highly effective. This is a very promising fact, as most cases of PHT in children are due to presinusoidal causes. However, in our study we had lesser number of cases with presinusoidal etiology, because most of these children present first with an upper gastrointestinal hemorrhage, which we had excluded. In our series, the response in children with sinusoidal etiologies though late, yet was statistically significant. But we noticed that the long term prognosis in sinusoidal PHTs was influenced more by the nature and progression of disease, rather than the specific management of portal hypertension. The findings of our study on b-blockers have been corroborated by similarreports in pediatric and adult patients.
[17,
18]
Lin et al
[19] substantiated in adult cirrhotic population that carvedilol with its fewer side effects has the potential to replace conventional propranolol for the prophylactic management of PHT. Tripathi et al
[20] also documented that carvedilol is an effective option for primary prophylaxis in patients with highrisk esophageal varices. The only previous study from our region on carvedilol was by De et al
[21] who monitored the acute effect of the drug in the form of reduction of hepatic venous pressure gradient (HVPG) in cirrhotic adult population. They documented that carvedilol is a relatively safe, effective portal hypotensive agent, both acutely and over 7 days, but not superior to propranolol. Our results corroborate with their observation even with longer follow-up.
Our major limitation was that we had to depend on indirect monitoring of portal venous pressure but this could be justified as efforts to directly measure venous pressure would have invited unnecessary ethical dilemmas in pediatric population. A relatively small sample size was another limitation of our study. We acknowledge that large multicentric trials evaluating our study protocol will be needed to validate our results, before applying them in general pediatric practice.
In summary, beta blockers are indeed effective in preventing variceal bleeds in children with portal hypertension. Our findings also suggest that carvedilol is a viable alternative to propranolol as its response rate is faster. But bearing in mind the cost of treatment coupled with the margin of efficacy over propranolol, carvedilol did not fare as a superior option over long term follow up.
Acknowledgements
We acknowledge the institutional ethics committee, NRS Medical College for giving us the necessary approval to carry out this study; and the Directorate of Science and Technology, Government of West Bengal, India for funding the study. The authors are grateful to Dr. A Bhowmick of Gastrointestinal Endoscopy Unit, Department of General Medicine, NRS Medical College and Hospital for performing the upper gastrointestinal endoscopies and Dr. M Karmakar of Department of Radiology, NRS Medical College and Hospital for performing the abdomen Doppler ultrasound of our patients.
References
- Alvarez F, Bernard O, Brunella F, Hadchouel P, Odièvre M,Alagille D. Portal obstruction in children. I. Clinical investigationsand hemorrhage risk. J Pediatr. 1983;103:696–702.
- Superina RA, Alonso EM. Medical and surgical management of portal hypertension in children. Curr Treat Options Gastroenterol. 2006;9:432–43.
- Celinska-Cedro D, Teisseyre M, Woynarowski M, Socha P, Socha J, Ryzko J. Endoscopic ligation of esophageal varices for prophylaxis of first bleeding in children and adolescents with portal hypertension: preliminary results of a prospective study. J Pediatr Surg. 2003;38:1008–11.
- Poddar U, Thapa BR, Rao KL, Singh K. Etiological spectrum of esophageal varices due to portal hypertension in Indian children: is it different from the West? J Gastroenterol Hepatol. 2008;23:1354–7.
- Gross M, Zoller WG. Medical prophylaxis of haemorrhage from oesophagealvarices in patients with liver cirrhosis. Eur J Gastroenterol Hepatol. 1997;9:603–12.
- Erkan T, Cullu F, Kutlu T, Emir H, Yesildag E, Sarimurat N, et al. Management of portal hypertension in children: a retrospective study with long-term follow-up. Acta Gastroenterol Belg. 2003;66:213–7.
- Yachha SK, Chetri K, Lal R. Management of portal hypertension. Indian J Pediatr. 2002;69:809–13.
- Conn HO. Ammonia tolerance in the diagnosis of eosophagealvarices. A comparison of endoscopic, radiologic and biochemical techniques. J Lab Clin Med. 1967;70:442–51.
- Sarin SK, Kumar A. Gastric varices: profile, classification, and management. Am J Gastroenterol. 1989;84:1244–9.
- Shashidhar H,LanghansN, Grand RJ. Propranolol in prevention of portal hypertensive hemorrhage in children: apilot study. J Pediatr Gastroenterol Nutr. 1999;29:12–7.
- Hemstreet BA. Evaluation of carvedilol for the treatment of portal hypertension. Pharmacotherapy. 2004;24:94–104.
- Kleber G, Ansari H, Sauerbruch T. Prophylaxis of first variceal bleeding. Baillieres Clin Gastroenterol. 1992;6:563–80.
- Zoller WG, Gross M. Beta-blockers for prophylaxis of bleeding from esophageal varices in cirrhotic portal hypertension. Review of the literature. Eur J Med Res. 1996;1:407–16.
- Shah VH, Kamath PS. Portal hypertension and Gastrointestinal bleeding. In: Fieldman M, Freidman LS, Brandt LJ, editors. Slesisenger and Fordtran's Gastrointestinal and liver Disease. 9th edition. Philadelphia :Saunders Elsevier; 2010.p.1502.
- Garcia-Tsao G, Bosch J, Groszmann RJ.Portal hypertension and variceal bleeding--unresolved issues. Summary of an American Association for the study of liver diseases and European Association for the study of the liver single-topic conference. Hepatology. 2008;47:1764–72.
- deFranchis R, Baveno V Faculty. Revising consensus in portal hypertension: report of the Baveno V consensus workshop on methodologyof diagnosis and therapy in portal hypertension. J Hepatol. 2010;53:762–8.
- Khanduri A, Yaccha SK, Kumar M. Etiologic spectrum of gastrointestinal bleeding in children- experience at a tertiary center. Indian J Gastroenterol. 1994;13:A3
- Lewis JA, Davis JM, Allsopp D, Cameron HA. Beta-blockers in portal hypertension. An overview. Drugs. 1989;37:62–9; discussion 74–6.
- Lin HC, Yang YY, Hou MC, Huang YT, Lee FY, Lee SD. Acute administration of carvedilol is more effective than propranolol plus isosorbide-5-mononitrate in the reduction of portal pressurein patients with viral cirrhosis. Am J Gastroenterol. 2004;99:1953–8.
- Tripathi D, Ferguson JW, Kochar N, Leithead JA, Therapondos G, McAvoy NC, et al. Randomized controlled trial of carvedilol versus variceal band ligation for the prevention of the first variceal bleed. Hepatology. 2009;50:825–33.
- De BK, Das D, Sen S, Biswas PK, Mandal SK, Majumdar D, et al. Acute and 7-day portal pressure response to carvedilol and propranolol in cirrhotics. J Gastroenterol Hepatol. 2002;17:183–9.