Obai Abdullah, Haythem Alabbas, Mohamed Abdel Khalek, Bernard M Jaffe, Emad Kandil
Division of Endocrine and Oncological Surgery
Department of Surgery, Tulane University School of Medicine,
1430 Tulane Ave, SL-22
New Orleans, LA 70112, USA
Corresponding Author:
Dr. Emad Kandil
Email: ekandil@tulane.edu
48uep6bbphidvals|480 48uep6bbph|2000F98CTab_Articles|Fulltext Retroperitoneal ganglioneuroma is a very rare entity especially in adolescents and adults. The relative rarity of this tumor in conjunction with lack of definite imaging findings, makes their diagnosis difficult to confirm. We present here a case of retroperitoneal ganglioneuroma, and suggest its consideration in the differential diagnosis of patients with abdominal pain.
Case Report
An 18 year old female presented with a chief complaint of intermittent, localized, non radiating left upper quadrant pain over a one week period. The pain was not related to food intake and she had no associated changes in bowel habits. She denied experiencing and nausea, vomiting, fever, chills, weight loss or other constitutional symptoms. The patient’s physical examination was unremarkable except for left upper quadrant tenderness without any peritoneal signs.
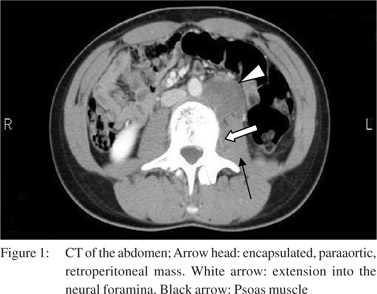
A computed tomography scan of her abdomen was performed which showed a heterogeneous, low density, left infrarenal paraaortic retroperitoneal mass along the anterior aspect of the iliopsoas muscle with extension to the adjacent third lumber vertebral body with no evidence of bone destruction. There was no evidence of lymphadenopathy (Figure 1).
Magnetic resonance imaging of the abdomen revealed a T1 hypointense, well encapsulated, left, paraaortic, retroperitoneal mass extending into the left L3 neural foramina, representing a neural origin. The patient was investigated for 24-hour urine catecholamine excretion rates and was found to be within normal limits.
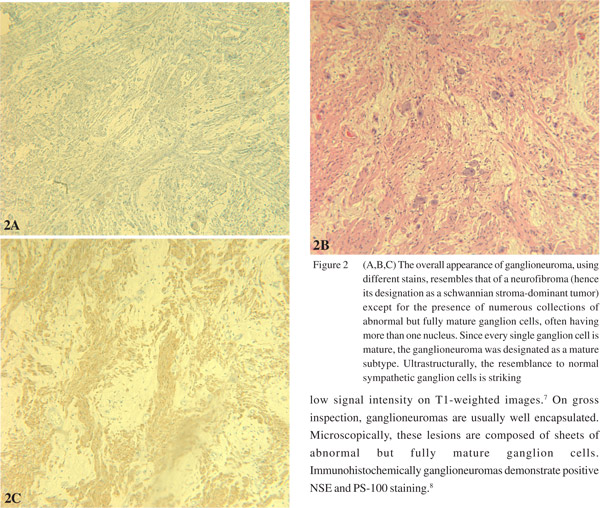
The patient underwent an uneventful exploratory laparotomy with excision of a well encapsulated mass measuring 6 × 4 × 2 cm. Histopathology examination revealed abnormal appearing ganglion cells and immunohistochemical stains were positive for NSE and S100. These findings were consistent with the diagnosis of ganglioneuroma (Figure 2a-c).
Discussion
Ganglioneuromas are benign neoplasms of the sympathetic nervous system of neuroectodermic origin and most often arise in the posterior mediastinum, retroperitoneum, adrenal medulla and pelvis.[1] They are very rare and effect newborns and infants more often than adolescents and adults.[2] Most ganglioneuromas are asymptomatic and diagnosed by chance. Rarely they are picked up because of their secretory activity, such as increased secretion of catecholamines.[3] However, compressive effects of the tumor on neighboring tissues may arise.[4,5] and cause abdominal pain. Rarely a palpable abdominal mass may be the only clinical finding.[6] Complete surgical excision is the treatment of choice.[4]
Ganglioneuromas have low, homogeneous attenuation on unenhanced CT scan and demonstrate slight to moderate enhancement which may be heterogeneous or homogeneous. On nuclear magnetic resonance imaging ganglioneuromas have low signal intensity on T1-weighted images.[7] On grossinspection, ganglioneuromas are usually well encapsulated. Microscopically, these lesions are composed of sheets of
abnormal but fully mature ganglion cells. Immunohistochemically ganglioneuromas demonstrate positive NSE and PS-100 staining.[8]
References
- Saikali S, Paumier V, Garrelon JL, Le Gall F. Facial primary cutaneous ganglioneuroma. Ann Pathol. 2009;29:138–41.
- Zugor V, Amann K, Schrott KM, Schott GE. Retroperitoneal ganglioneuroma. Aktuelle Urol. 2005;36:349–52.
- Bunn ND Jr, King AB. Cervical ganglioneuroma. A case report and review of the literature. Guthrie Clin Bull. 1961;30:5–14.
- Geoerger B, Hero B, Harms D, Grebe J, Scheidhauer K, Berthold F. Metabolic activity and clinical features of primary ganglioneuromas. Cancer. 2001;91:1905–13.
- Hayes FA, Green AA, Rao BN. Clinical manifestations of ganglioneuroma. Cancer. 1989;63:1211–4.
- Cai J, Zeng Y, Zheng H, Qin Y, T K, Zhao J. Retroperitoneal ganglioneuroma in children: CT and MRI features with histologic correlation. Eur J Radiol. 2010;73:315–20.
- Guo YK, Yang ZG, Li Y, Deng YP, Ma ES, Min PQ, et al. Uncommon adrenal masses: CT and MRI features with histopathologic correlation. Eur J Radiol. 2007;62:359–70.
- Domanski HA. Fine-needle aspiration of ganglioneuroma. Diagn Cytopathol. 2005;32:363–6.
- Karaosmanoglu D, Karcaaltincaba M, Oguz B, Akata D, Ozmen M, Akhan O. CT findings of lymphoma with peritoneal, omental and mesenteric involvement: peritoneal lymphomatosis. Eur J Radiol. 2009;71:313–7.
- Nishino M, Hayakawa K, Minami M, Yamamoto A, Ueda H, Takasu K. Primary retroperitoneal neoplasms: CT and MR imaging findings with anatomic and pathologic diagnostic clues. Radiographics. 2003;23:45–57.
- Spillane AJ. Retroperitoneal sarcoma: time for a change in attitude? ANZ J Surg. 2001;71:303–8.
- Feng N, Zhang WY, Wu XT. Clinicopathological analysis of paraganglioma with literature review. World J Gastroenterol. 2009;15:3003–8.
- Conti P, Mouchaty H, Spacca B, Buccoliero AM, Conti R. Thoracic extradural paragangliomas: a case report and review of the literature. Spinal Cord. 2006;44:120–5.
|