Sujata Siwat offshorech1, Mohd Talha Noor2, Usha Dutta2, Rakesh Kochhar2, Arunanshu Behera3, Kartar Singh2
Departments of Obstetrics & Gynecology,1
Gastroenterology2 and Surgery3
Postgraduate Institute of Medical Education and Research,
Chandigarh - 160012, India
Corresponding Author:
Dr. Sujata Siwatch
Email: ssiwatch@hotmail.com
48uep6bbphidvals|482 48uep6bbph|2000F98CTab_Articles|Fulltext Bowel obstruction is uncommon during pregnancy. It was first reported by Houston in 1830.[1] The incidence of intestinal obstruction during pregnancy (IOP) ranges from 1 in 1500 to 1 in 66,431 pregnancies in various case series.[2,3] Small bowel volvulus, however, is very rare and represents less than 2% of all cases of IOP. We present an unusual case of small bowel obstruction secondary to midgut volvulus with underlying malrotation during pregnancy managed endoscopically with successful outcome of pregnancy.
Case Report
A 23 year old primigravida at 20 weeks of gestation presented with 5 days history of sudden onset upper abdominal colicky pain with recurrent episodes of bilious vomiting. There was no obstipation or abdominal distension. She had no previous history of pain abdomen or abdominal surgery. She had had an uneventful pregnancy till then and there was no history of vomiting in the first trimester.
Patient on evaluation was dehydrated, afebrile, and had blood pressure of 90/60 mmHg. Abdominal examination revealed epigastric tenderness. Gynecological examination revealed uterine size corresponding to 20 weeks of gestation and fetal heart pattern was reactive. Laboratory studies showed
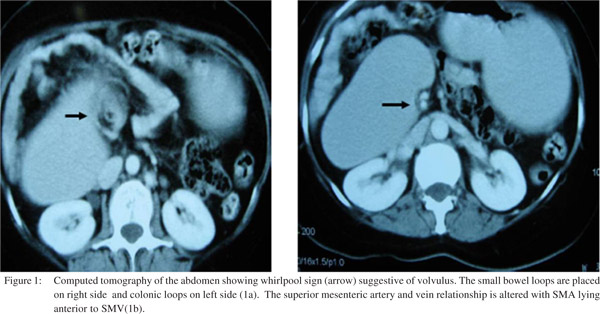
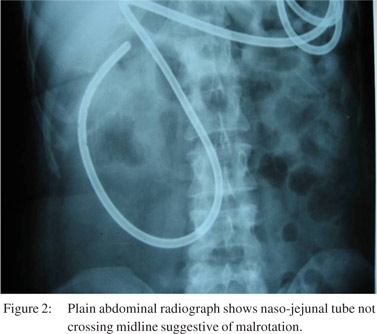
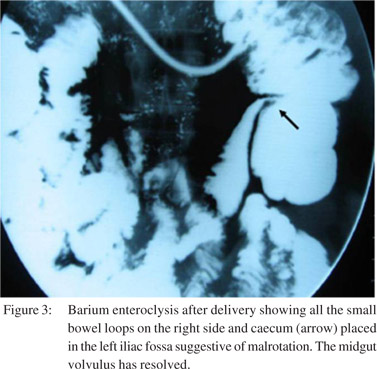
hypokalemia, normal leukocyte count, increased transaminases and urinary ketones were positive. Initial possibilities of either hyperemesis gravidarum or anicteric hepatitis (her serum ALT and AST were elevated more than 3 times) was entertained and patient was managed on standard treatment but witnessed no improvement in her symptoms. Her viral markers were negative for hepatitis A, B, C and E viruses. With supportive care her biochemical parameters normalized, however vomiting persisted. Upper gastrointestinal endoscopy (UGIE) showed dilated stomach and proximal duodenum with excessive bile stained residue. Considering the possibility of intestinal obstruction, she was subjected to contrast enhanced computerized tomography (CECT) of abdomen which revealed dilated stomach, first and second part of duodenum (D1 & D2), with obstruction beyond D2 secondary to volvulus with evidence of malrotation (Figure 1). Enteroscopy was performed which showed dilated stomach, first and second part of duodenum (D1, D2), with an abruptly short twisted segment at second and third part of duodenum (D2, D3) with normal mucosa. Scope was negotiable with difficulty across the site and a guide-wire was negotiated across the narrowing over which a naso-jejunal feeding tube was passed beyond the obstruction. Patient was started on balanced naso-jejunal feeding (2400 kcals/day). She tolerated jejunal feeds and remained asymptomatic. Surgical opinion was sought and surgery was considered to be a high risk intervention in view of her poor general condition and gestation. In view of no evidence of bowel ischemia or signs of peritonism it was decided to manage the patient conservatively. Fetal monitoring was done at regular intervals which showed normal intrauterine growth. The patient went into spontaneous labor at 34 weeks of gestation and delivered a healthy baby with no evidence of congenital malformations. Two weeks post delivery the patient was taken up for small bowel barium examination which showed malrotation but the volvulus had spontaneously resolved post delivery (Figures 2,3). The patient was subsequently discharged. Three years after her delivery she developed symptoms suggestive of biliary colic for which she underwent evaluation and was found to have multiple gallstones. At surgery the duodenal flexure was noted to the right side of origin of superior mesenteric artery, cecocolic junction to the left side of origin superior mesenteric artery, Ladd’s bands from retroperitoneum to cecocolic junction across duodenum and multiple gallstones. She underwent open cholecystectomy and Ladd’s procedure and appendicectomy. She has recovered uneventfully in her postoperative period and doing well. Her child is now 3 years old and also doing well.
 Discussion
Intestinal obstruction is rare during pregnancy. However, it is associated with high maternal and fetal morbidity and mortality.[4] Several factors lead to delay in diagnosis. Recurrent vomiting may be attributed to hyperemesis gravidarum. Averting radiological investigations due to perceived risk of radiation injury to growing fetus, results in delay in diagnosis. Adhesions are the commonest cause of intestinal obstruction of pregnancy (IOP) and are seen in 60% of cases,[5] followed by volvulus in 25% of cases.. Other causes include intussusception (5%), carcinoma (3.5%), hernia (1.5%), and appendicitis (0.5%).[4] Small bowel volvulus represents only 1- 3% of all cases of IOP. Small bowel volvulus especially secondary to malrotation is extremely rare.
Discussion
Intestinal obstruction is rare during pregnancy. However, it is associated with high maternal and fetal morbidity and mortality.[4] Several factors lead to delay in diagnosis. Recurrent vomiting may be attributed to hyperemesis gravidarum. Averting radiological investigations due to perceived risk of radiation injury to growing fetus, results in delay in diagnosis. Adhesions are the commonest cause of intestinal obstruction of pregnancy (IOP) and are seen in 60% of cases,[5] followed by volvulus in 25% of cases.. Other causes include intussusception (5%), carcinoma (3.5%), hernia (1.5%), and appendicitis (0.5%).[4] Small bowel volvulus represents only 1- 3% of all cases of IOP. Small bowel volvulus especially secondary to malrotation is extremely rare.
Patients with malrotation are at an increased risk of presenting with volvulus during pregnancy due to displacement of bowel loops by the gravid uterus. This is especially true during 16 to 20 weeks and 32 to 36 weeks or during puerperium when rapid changes in uterine size occur. Volvulus results in partial obstruction of the small intestine with proximal distension and torsion at the point of fixation.[6] Factors predisposing to volvulus include post operative adhesions, Ladd’s bands and malrotation.[4,7]
Surgical resection for volvulus is the preferred treatment, as it eliminates the risk of recurrence and decreases morbidity and mortality.[8] Detorsion has also been suggested as an option if the bowel has not undergone necrosis and ischemia, however there remains a risk of recurrence. In our patient, the nasojejunal tube placed across the site of torsion not only provided a means to deliver nutrition, it also functioned as a splint to prevent recurrent rotation of the gut at this site. We have previously reported use of naso-jejunal tube placement as a splint to treat retrograde jejuno-gastric intussusceptions.[9,10] This case highlights endoscopic management of IOP secondary to malrotation with partial volvulus during pregnancy with successful outcome. This is the first case in published literature where pregnancy with malrotation and a volvulus was treated successfully non-surgically using a nasoenteric tube for feeding cum stenting.
Early establishment of definitive diagnosis even if it involves radiation exposure is key in organizing management of such problems during pregnancy. Risk of maternal and fetal mortality associated with intestinal obstruction outweighs the potential risk of fetal radiation exposure. Fetal risk is considered to be negligible at exposures of 5 rad or less when compared to the risks of intestinal obstruction during pregnancy. The radiation exposure with plain X-ray is only 0.1 rad and with CT scan it is 2.6 rad both of which are within the safe limits of radiation exposure during pregnancy.[11]
References
- Houston J. Intestinal obstruction in the fourth month of pregnancy due to adhesions. J Iowa Med Soc. 1941;31:237.
- Ballantyne GH, Brandner MD, Beart RW Jr, Ilstrup DM. Volvulus of the colon. Incidence and mortality. Ann Surg. 1985;202:83–92.
- Beck WW Jr. Intestinal obstruction in pregnancy. Obstet Gynecol. 1974;43:374–8.
- Connolly MM, Unti JA, Nora PF. Bowel obstruction in pregnancy. Surg Clin North Am. 1995;75:101–3.
- Perdue PW, Johnson HW Jr, Stafford PW. Intestinal obstruction complicating pregnancy. Am J Surg. 1992;164:384–8.
- Goldthorp WO. Intestinal obstruction during pregnancy and puerperium. Br J Clin Pract. 1966;20:367–76.
- Ventura-Braswell AM, Satin AJ, Higby K. Delayed diagnosis of bowel infarction secondary to maternal midgut volvulus at term. Obstet Gynecol. 1988;91:808–10.
- Sherer DM, Abulafia O. Postcesarean small bowel volvulus. Case report and review of the literature. Gynecol Obstet Invest. 2001;51:69–72.
- Kochhar R, Saxena R, Nagi B, Gupta NM, Mehta SK. Endoscopic management of retrograde jejunogastric intussuception. Gastrointest Endosc. 1988;34:56–7.
- Saxena R, Kochhar R, Nagi B, Mehta SK, Gupta NM. Nonsurgical treatment of jejunogastric intussusception. Surg Endoscopy. 1988;2:88–91.
- Toppenberg KS, Hill DA, Miller DP. Safety of radiographic imaging during pregnancy. Am Fam Physician.1999;59:1813–8, 1820.
|