Ashish Kumar Jha, Rupesh Pokharna, Sandeep Nijhawan, Arya Suchismita
Department of Gastroenterology,
SMS Medical College, Jaipur, India
Corresponding Author:
Dr. Ashish Kumar Jha
Email: ashishjhabn@yahoo.co.in
48uep6bbphidvals|503 48uep6bbph|2000F98CTab_Articles|Fulltext The close topographic relationship between pancreas and the upper abdominal organs causes alterations of the surrounding internal milieu in patients with chronic pancreatitis (CP). In primary asymptomatic CP, local complications may be the first clue to pancreatic disorders. Involvement of the colon is unusual in pancreatitis and can have serious sequelae. In a study, 6.1% of patients referred for surgical management of pancreatitis had colonic complications.[1] Colonic complications are more frequent in severe disease, occurring in up to 15% of severe pancreatitis.[2] Colonic stenosis has been described in 7% of acute pancreatitis, 1.5% of CP and an overall prevalence of 2 to 6.1%.[1,3] There are few studies reporting prevalence of colonic strictures (CS) in pancreatitis from India.[4] Asymptomatic CP presenting as CS is extremely rare.[5,6] We describe here a complication of painless CP presenting as acute intestinal obstruction due to CS.
Case report
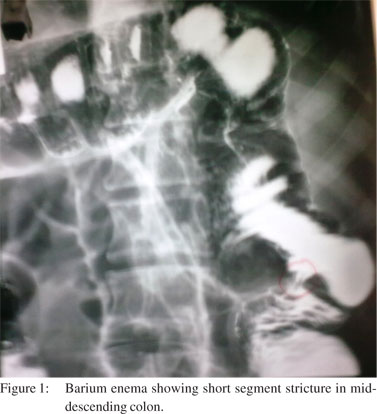
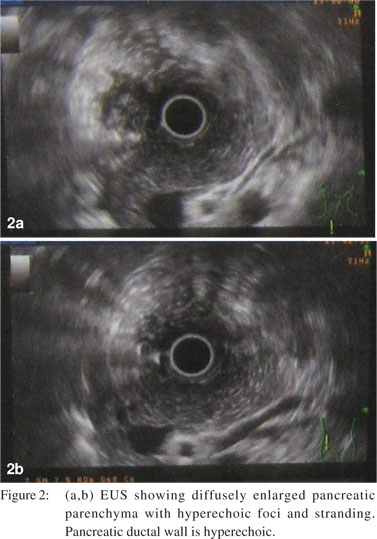
A 35-year-old male presented with history of recent onset constipation since 5 months. Over last 4 days he had developed moderate colicky pain abdomen, progressive abdominal distension and obstipation. He was a chronic alcoholic, consuming approximately 240 ml of whisky a day. Two years back he had a mild episode of acute alcoholic pancreatitis. On examination his vital parameters were normal, he had pallor, his abdomen was distended, soft, with mild tenderness in the left upper quadrant and epigastrium. Bowel sounds were exaggerated. Blood analysis revealed hemoglobin of 10.5 gm/ dl and normal total leukocyte count. Blood sugar, renal and liver function tests were normal. Serum amylase and lipase levels were also normal. Chest radiographs were normal, however, abdominal plain radiographs showed dilated large bowel loop with multiple air-fluid levels. Abdominal ultrasonography showed gaseous abdomen with dilated bowel loops. The patient was placed on conservative treatment for acute large bowel obstruction. Colonoscopy revealed luminal stenosis at descending colon with normal mucosa with scope not negotiable further. Barium enema revealed short segment stricture in mid-descending colon (Figure 1). Abdominal computed tomography (CT) showed circumferential thickening of mid-descending colon without any evidence of mass lesion or extrinsic compression. The pancreas appeared normal. The patient underwent laparotomy which revealed retroperitoneal calcification in and around the splenic flexure and in the colonic mesentery. A small focus of necrosis was also noted in the tail of pancreas. He had a stricture at the splenic flexure and in the adjacent descending colon. A transverse-sigmoid bypass with necrosectomy was thus performed with satisfactory recovery thereafter. Histopathology examination of the resected specimen revealed nonspecific chronic inflammatory cells with fibrosis. However, no evidence of granuloma, caseation necrosis, acid fast bacilli or malignant cells was found. PCR for tuberculosis was negative. In view of chronic alcohol intake, prior acute pancreatitis and intra-operative findings, endoscopic ultrasonography (EUS) of pancreas was advised, which revealed diffusely enlarged pancreatic parenchyma with hyperechoic foci and stranding (Figure 2). There was an oval hyperechoic area of 7 mm diameter, possibly due to fibrotic strands in the head region. Pancreatic ductal wall was hyperechoic. The
patient was advised to abstain from alcohol. He is doing well at six month follow-up.
 Discussion
The colonic complications of pancreatitis include localized paralytic ileus, necrosis, perforation, hemorrhage, fistulae, stenosis and pseudocyst compressing or eroding into the adjacent colonic segment.[1-3,7] The nature of complications depends on the severity and duration of pancreatitis, anatomical relationship of the colonic segment to the pancreas and other associated complications of pancreatitis like abscess formation.[2,3,7] Colonic stenosis can either manifest early due to necrosis, ischemia and formation of an inflammatory mass or can present months to years after the inciting episode of pancreatitis consequent to retraction of the colon or by compression by a pancreatic pseudocyst or as a consequence of pericolic fibrosis.[3,5,7] Hunt and Mildenhall[7] have postulated that mesenteric ischaemia associated with a severe attack of pancreatitis may lead to fibrosis and stricture formation in the long term. Pancreatic carcinoma invading the colon has also been described in a patient of CP.[5] Enzymatic, inflammatory and ischemic processes are believed to be involved in the pathogenesis of colonic complications.[7,8]
Discussion
The colonic complications of pancreatitis include localized paralytic ileus, necrosis, perforation, hemorrhage, fistulae, stenosis and pseudocyst compressing or eroding into the adjacent colonic segment.[1-3,7] The nature of complications depends on the severity and duration of pancreatitis, anatomical relationship of the colonic segment to the pancreas and other associated complications of pancreatitis like abscess formation.[2,3,7] Colonic stenosis can either manifest early due to necrosis, ischemia and formation of an inflammatory mass or can present months to years after the inciting episode of pancreatitis consequent to retraction of the colon or by compression by a pancreatic pseudocyst or as a consequence of pericolic fibrosis.[3,5,7] Hunt and Mildenhall[7] have postulated that mesenteric ischaemia associated with a severe attack of pancreatitis may lead to fibrosis and stricture formation in the long term. Pancreatic carcinoma invading the colon has also been described in a patient of CP.[5] Enzymatic, inflammatory and ischemic processes are believed to be involved in the pathogenesis of colonic complications.[7,8]
The most common site of colonic stenosis is at or around the splenic flexure probably due to anatomical proximity to the tail of pancreas. However involvement of other sites is also reported.[3] Colonic stenosis frequently presents with intestinal obstruction. It can also mimic inflammatory bowel disease (IBD), malignancy, tuberculous stricture and nonsteroidal antiinflammatory drugs (NSAIDS) induced CS.[6,9,10] Asymptomatic CP presenting as CS has been described in few case reports and poses a diagnostic challenge.[5,6] Barium enema is a good modality to diagnose CS however, in atypical presentation other imaging modalities and histopathology examination of stricture tissue is warranted. In recent years EUS has emerged as a more sensitive tool than conventional tests like ERCP, CT scan and MRCP in diagnosing CP.[11] In this case CT scan had failed however, EUS detected early changes of CP. Therefore, in cases of unexplained inflammatory CS with a high clinical suspicion of pancreatitis, undertaking EUS may prove rewarding. Patients of CS due to a complication of pancreatitis usually have good prognosis after surgery, as we seen in our patient.[3,6]
Our patient was a chronic alcoholic, and had had a prior episode of acute alcoholic pancreatitis. He presented with acute large bowel obstruction due to CS and on evaluation underlying asymptomatic CP was found. There was no other obvious causative factor which could have incited the colonic stenosis. Presence of calcification surrounding the stricture segment and histopathological evidence of chronic inflammatory cells with fibrosis in the resected specimen suggest a chronic inflammatory process as the possible mechanism for stricture formation. CP or prior episode of acute pancreatitis (acute on chronic pancreatitis) could be the cause of necrosis and subsequent chronic inflammatory reaction.
References
- Adams DB, Davis BR, Anderson MC. Colonic complications of pancreatitis. Am Surg. 1994;60:44–9.
- Mohamed SR, Siriwardena AK. Understanding the colonic complications of pancreatitis. Pancreatology. 2008;8:153–8.
- Fékété F, Rongère C. Colonic stenosis in pancreatitis. Ann Gastroenterol Hepatol. 1985;21:363–4.
- Baig SJ, Rahed A, Sen S. A prospective study of the aetiology, severity and outcome of acute pancreatitis in Eastern India. Trop Gastroenterol. 2008;29:20–2.
- Gardner A, Gardner G, Feller E. Severe colonic complications of pancreatic disease. J Clin Gastroenterol. 2003;37:258–62.
- Pascual M, Pera M, Martínez I, Miquel R, Grande L. Intestinal occlusion due to pancreatitis mimicking stenosing neoplasm of the splenic angle of the colon. Gastroenterol Hepatol. 2005;28:326–8.
- Negro P, D’Amore L, Saputelli A Talarico C, Scaccia M, Tuscano D, Gossetti F et al. Colonic lesions in pancreatitis. Ann Ital Chir. 1995;66:223–31.
- Hunt DR, Mildenhall P. Etiology of strictures of the colon associated with pancreatitis. Am J Dig Dis. 1975;20:941–6.
- Hancock RJ, Christensen RM, Osler TR, Cassim MM. Stenosis of the colon due to pancreatitis and mimicking carcinoma. Can J Surg. 1973;16:393–8.
- Greiner L. Colonic stenosis following chronic pancreatitis. Rare differential diagnosis of Crohn’s regional colitis. Med Welt. 1982;33:1632–3.
- Morris-Stiff G, Webster P, Frost B, Lewis WG, Puntis MC, Roberts SA. Endoscopic ultrasound reliably identifies chronic pancreatitis when other imaging modalities have been non-diagnostic. JOP. 2009;10:280–3.
|