John Menache offshorery1, Yogesh Chawla1, Arunaloke Chakrabarti2, Ajay Duseja1, Radha Dhiman1, Naveen Kalra3
Departments of Hepatology,1 Microbiology2 and
Radiodiagnosis,3
Postgraduate Institute of Medical Education and Research,
Chandigarh, India.
Corresponding Author:
Dr. YK Chawla
Email : ykchawla@gmail.com
48uep6bbphidvals|544 48uep6bbph|2000F98CTab_Articles|Fulltext Most of the liver abscesses in developing countries are amoebic or pyogenic in origin. Fungal liver abscesses are uncommon and are usually diagnosed in immunocompromised patients. We describe the occurrence of a fungal liver abscess in a young immunocompetent man.
Case report
A 30-year-old man presented with abdominal pain since 3 days. Physical examination was unremarkable except for mild tenderness in the right upper quadrant of the abdomen. He had no fever and there was no past history of recurrent infections. His blood counts and fasting blood sugar levels were normal. ELISA for human immunodeficiency virus was negative on two occasions and his absolute CD4+ cell count
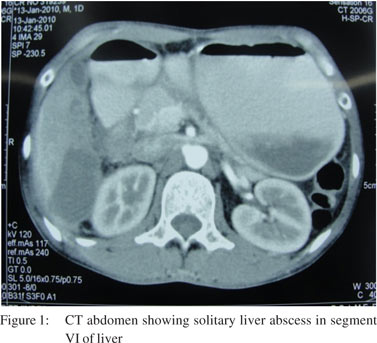
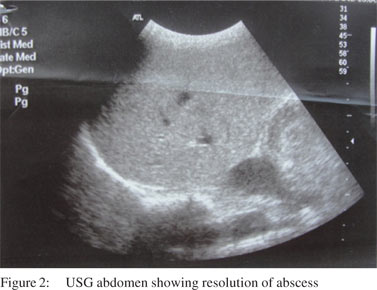
was within normal limits. His abdominal ultrasound showed a 5 cm × 4 cm abscess in segment VI of the liver, which was subsequently confirmed on CT scan (Figure 1). His amoebic serology and hydatid serology were negative. The aspirate from the abscess showed no bacterial growth, but revealed yeast cells with pseudohyphae on direct microscopy and grew Candida albicans after four days. His blood cultures were sterile. Five days later the abscess was reassessed and re-aspirated to yield a similar picture on direct microscopy and grew C. albicans. He was diagnosed to have Candidial liver abscess and was prescribed oral fluconazole 200 mg BD for 6 weeks as the organism was found to be sensitive to the drug. His pain subsided with treatment and an abdominal ultrasound done two months later showed complete resolution of the abscess (Figure 2).
 Discussion
Our patient was a young male with a large solitary liver abscess. Amoebic liver abscess would have been the expected clinical diagnosis with this presentation. However amoebic serology was negative and the cultures from the abscess cavity repeatedly grew Candida albicans without any sign of bacterial growth, thus leading us to the diagnosis of a Candidial liver abscess. The gastrointestinal tract appears to be the
probable source of the Candida infection in this patient.
To the best of our knowledge, this is only the second instance of a fungal liver abscess reported in an immunocompetent host. In an earlier report Candida glabrata liver abscess was discovered in a 64-year-old female, but that patient had chronic obstructive pulmonary disease and had received multiple antibiotics as well as short duration steroid therapy.[1] In contrast our patient did not have any long standing illness and had never been on any immunosuppressant medication. Most hepatic fungal abscesses occur in patients with hematological malignancies and are caused by Candida albicans.[2] Marcus et al, observed that 19 of 20 fungal abscesses in cancer patients were caused by Candida albicans. Fifteen of them had hematologic malignancies.[3]
The patient responded to fluconazole. The current IDSA clinical practice guidelines on the management of candidiasis also recommend fluconazole as the initial therapy for invasive candidiasis caused by C. albicans in non-neutropenic adults.[4] The fact that the patient was immunocompetent may have some bearing on the unusual clinical presentation and excellent response to treatment that was seen in this patient. Our report suggests that it will be prudent to exclude fungal infections in case the bacterial cultures are sterile from a pyogenic abscess as attempts to treat can be quite rewarding.
References
Discussion
Our patient was a young male with a large solitary liver abscess. Amoebic liver abscess would have been the expected clinical diagnosis with this presentation. However amoebic serology was negative and the cultures from the abscess cavity repeatedly grew Candida albicans without any sign of bacterial growth, thus leading us to the diagnosis of a Candidial liver abscess. The gastrointestinal tract appears to be the
probable source of the Candida infection in this patient.
To the best of our knowledge, this is only the second instance of a fungal liver abscess reported in an immunocompetent host. In an earlier report Candida glabrata liver abscess was discovered in a 64-year-old female, but that patient had chronic obstructive pulmonary disease and had received multiple antibiotics as well as short duration steroid therapy.[1] In contrast our patient did not have any long standing illness and had never been on any immunosuppressant medication. Most hepatic fungal abscesses occur in patients with hematological malignancies and are caused by Candida albicans.[2] Marcus et al, observed that 19 of 20 fungal abscesses in cancer patients were caused by Candida albicans. Fifteen of them had hematologic malignancies.[3]
The patient responded to fluconazole. The current IDSA clinical practice guidelines on the management of candidiasis also recommend fluconazole as the initial therapy for invasive candidiasis caused by C. albicans in non-neutropenic adults.[4] The fact that the patient was immunocompetent may have some bearing on the unusual clinical presentation and excellent response to treatment that was seen in this patient. Our report suggests that it will be prudent to exclude fungal infections in case the bacterial cultures are sterile from a pyogenic abscess as attempts to treat can be quite rewarding.
References
- Lima R, Shams W, Kalra S, Borthwick T. Candida glabrata liver abscess and fungemia complicating severe calculus cholecystitis in an immunocompetent nondiabetic host. South Med J. 2010;103:245–7.
- Ralls PW. Inflammatory diseases of the liver. Clin Liver Dis. 2002;6:203–25.
- Marcus SG, Walsh TJ, Pizzo PA, Danforth DN Jr. Hepatic abscess in cancer patients. Characterization and management. Arch Surg. 1993;128:1358–64; discussion 1364.
- Pappas PG, Kauffman CA, Andes D, Benjamin DK Jr, Calandra TF, Edwards JE Jr, et al. Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clin Infectious Dis. 2009;48:503–35.
|