Vijay Ramachandran1, Abdul Rahman Hyder2, Undemane Shivashankara Vinayaka3, Devdas Acharya4
Department of Surgical Gastroenterology1, Radiology3,4,
Yenepoya Medical College, Deralakatte, and
Department of Medical Gastroenterology2, Mangalore,
Karnataka.– 575018
Corresponding Author:
Dr. Vijay Ramachandran
Email: drvijayr@gmail.com
48uep6bbphidvals|598 48uep6bbph|2000F98CTab_Articles|Fulltext Patients with neurofibromatosis type 1 (Von Recklinghausen’s disease, NF 1) suffer from cutaneous, neurological and intestinal manifestations due to the mutation of the neurofibromin gene and the abnormal protein product. Patients with NF 1 are prone to developing gastrointestinal stromal tumours (GIST). We report the case of successful laparoscopic-assisted small bowel resection of multiple small bowel GISTs in a patient with NF 1.
Case report
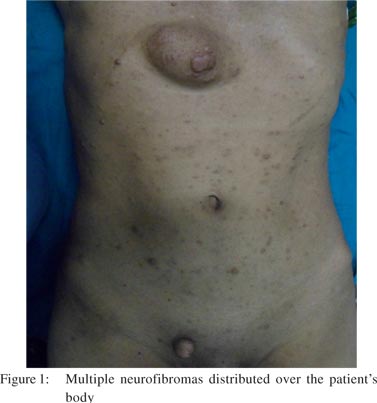
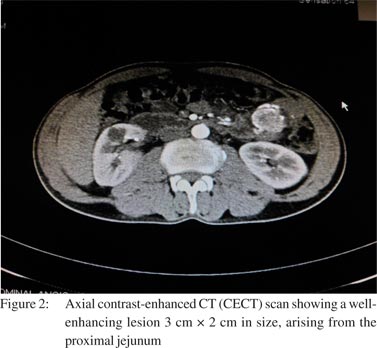
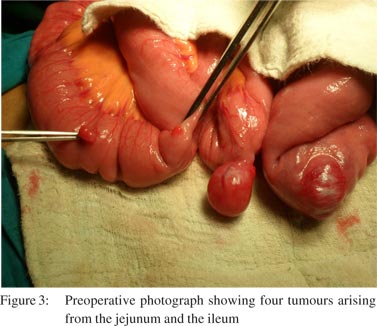
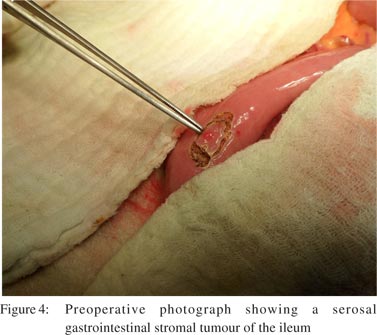
A 42-year-old man presented with recurrent episodes of melaena of 2 weeks’ duration. The patient denied history of ingestion of alcohol or medications. Clinical examination was unremarkable except for multiple cutaneous neurofibromas, axillary freckles and cafe au lait spots (Figure 1). Haematological tests revealed microcytic hypochromic anaemia and faecal occult blood was positive. Both upper GI endoscopy (UGIE) and colonoscopy were normal. CT angiogram of the abdomen (Figure 2) revealed the presence of two masses 3 cm × 2 cm in size, enhancing well with contrast, located in the proximal and mid jejunum and supplied by branches of the superior mesenteric artery. After obtaining an informed consent and preoperative packed cell transfusions, the patient was taken up for diagnostic laparoscopy. Findings at laparoscopy included two jejunal tumours as described above and additional three lesions 1 cm × 1 cm in size, located on the ileal serosa (Figures 3 and 4). Laparoscopic-assisted extracorporeal small bowel resection and anastomoses (three), full thickness excision of a non-contiguous serosal GIST and repair of defect in two layers was done. Histopathology of the resected specimen revealed well circumscribed, spindle cell proliferation with minimal atypia and rare mitoses. Immunostaining was positive for CD117. The postoperative period was uneventful and the patient was discharged on postoperative day 7. No adjuvant treatment was given and the patient is asymptomatic at 2 months’ follow-up.
Discussion
Abdominal involvement in NF 1 includes GIST, phaeochromocytoma and ampullary tumours. c-KIT mutations, which are found in 78% of sporadic GISTs, are rarely seen in NF 1-associated tumours.[1,2] This has potential implications as imatinib therapy is likely to be ineffective in c-KIT-negativetumours.[1] This case also highlights the utility of laparoscopicassisted small bowel resection of multiple small bowel GISTs in a patient with NF 1.[2]
References
- Aboutaleb E, Kothari M, Damrah O, Canelo R. c-KIT positive astrointestinal stromal tumor presenting with acute bleeding in a patient with neurofibromatosis type 1: a case report. Int Semin Surg Oncol. 2009;6:17.
- Tsukuda K, Ikeda E, Takagi S, Miyake T, Muraoka T, Watanabe K, et al. Multiple gastrointestinal stromal tumors in neurofibromatosis type 1 treated with laparoscopic surgery. Acta Med Okayama. 2007;61:47–50.
|